What Is Basal Insulin?
The main job of basal insulin (also known as long-acting insulin or the basal rate in your pump) is to keep your blood sugar at a consistent level when you’re not eating. It’s important to get your basal rate set correctly because it’s the foundation of your diabetes regimen. And once you get your basal rate figured out, it usually doesn’t change very much over time.
How Do You Know If Your Basal Rate Is Set Correctly?
The best way to test your basal rate is to do it overnight. Decide on the night that you’re going to test – you don’t want to do it on a night that you’re going to be exercising late, eating late, or staying up later than usual.
The night of the test, try to have an early dinner around 5:00 or 6:00 pm. After dinner, don’t eat anything more. You want your post-meal blood sugar in a desirable range (between 140-180 mg/dL) and you want it to be steady. If your post-meal blood sugar is above 200, give a little correction dose so by the time you go to bed, you’re flat. If you’re on a CGM, your trend arrow should be horizontal at bedtime. Check your blood sugar before you fall asleep, and write the number down if you need to so you don’t forget.
If you’re not on a CGM, plan on testing your blood sugar every few hours throughout the night, or at least once around 3:00 am. Important update for you type 2s – CGM is now approved by Medicare and other insurance companies if you are on one shot of basal insulin! Previously you had to be on three shots a day to be eligible to receive coverage for a CGM.
When you wake up in the morning, check your blood sugar again. If your basal rate is set correctly, you should wake up with nearly the same blood sugar you went to bed with, give or take 30 points. So if you went to bed at 150 mg/dL, you should wake up between 120-180 mg/dL.
Keep an Eye Out for Patterns
You can do this test a few times to see if you notice a pattern. If you’re consistently going to bed at 150 and waking up at 250, that means you’re not getting enough basal insulin. If your numbers are creeping down overnight, that means you may be on too much basal insulin. In either case, you should speak with your provider about adjusting your basal rate.
What if you go to bed at 250 and you wake up at 250? Do you need to increase your basal rate?
Trick question! The answer is no. If you’re going to bed at 250 and you’re waking up at 250, your blood sugar is flat. Your basal is doing its job. The problem is that you’re going to bed too high, so you need to take more mealtime insulin with dinner so you go to bed closer to 150 with a horizontal trend arrow.
How Often Should You Test Your Basal Rate?
If you have type 1 or type 2 diabetes and you’re on basal insulin, you should test your basal rate at least once a year. It’s a simple thing to do, and it really pays dividends in your overall diabetes management.
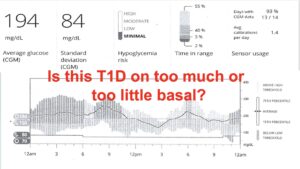
A Real-Life Case Study
The download below is from a patient of mine who was having some trouble with glucose control. His standard deviation was very high starting at midnight, but it’s not possible to tell from the download if he was on too much or too little basal, so I decided to put him through the test.
It’s a little hard to appreciate the slope of the overnight glucose line from the next image below, but between midnight and 6:00 am he went from 150 mg/dL to 100 mg/dL. That’s a drop of 50 points, so he was definitely on too much basal insulin.
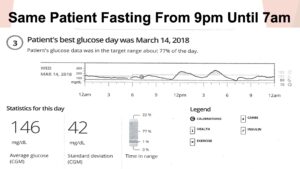
Many providers’ first thought after seeing the first image with the overnight high standard deviation would be to increase the patient’s basal insulin, but in actuality what he needed was less basal insulin. This patient was doing a lot of late-night snacking and not blousing, so that was the issue that we were able to address.
The Takeaway
Remember, if you are using a pump that delivers a basal rate or you take a long-acting basal insulin such as Lantus, Tresiba, or Toujeo, make sure you are getting the right amount to stay flat in the fasting state like overnight and in between widely spaced meals. Having a good basal dose is an important foundation to build upon.
Additional Resources:
Overbasalization in Type 1 and Type 2 Diabetes: You Can Have Too Much of a Good Thing!


Based on this blog I decided to Basel test last night. But I’m on CIQ. I currently have different basil profile set throughout the night because I do tend to drop low. I started at 10:30 at 1:29 and at 8:30 this morning I was 136. However when I looked at my tconnect, I did go up for a while in the middle of the night. Is that OK?
Totally OK…sounds like a good test. FYI if you are on the CIQ you should not need too many basal rates. Most of my patients have one as the system will modulate your basal rate depending on predicted CGM value.
So if my Basel rate is correct, once all my bolus is out of my system between a meals, my blood sugar should stay fairly level, correct? Mine starts to climb as soon as my bolus has run it’s course. I use MDI. When I did an overnight Basel test 6 is too low and 7 is a bit too much. Thoughts? I would really appreciate any input. I am coming to The One Confrence as well and can’t wait.
To answer your first question, yes your blood sugar should stay fairly level as long as you’re not doing unusual exercise. For your second question, giving insulin with a pen is hard to give accurate doses that low. You could get the 25 or 30-unit syringes where you can give an accurate .5 dose, so you could give yourself 6.5. If your insulin does not come in a vial, you can suck it out of the pen itself.
Humalog Jr is a half-unit pen. NovoPen Echo is a half-unit pen that uses cartridges and the Medtronic InPen also doses in half units.
Just realized that she need Hal-unit basal – not rapid acting!! Please disregard my last post – half-unit syringes are the way to go!! (Need my morning coffee)
Haha! No problem Sarah – thanks for the clarification!
Hi Dr Edelman, I found this article very interesting! I have a query – my glucose levels are stable over night but they’re stable between 4.4 and 5.6. Firstly, I’m curious to know if you feel that being in the low 4s is too low during the night, bearing in mind I have not had a reading below 4. Secondly, if I wanted my level to be stable but a bit higher (ideally at a minimum of above 5 let’s say), would the basal need to be reduced or would I achieve that by adjusting my evening meal bolus? I am experimenting with this at the moment but thought I’d see if you had any thoughts as I’m rather new to this. Many thanks.
Hi Elizabeth,
To answer your first question…yes, you’re definitely too low at night. There’s no need to be that low. It’s just going to cause you problems, and you’re not even in the range of causing any complications. You can get into serious problems on occasion if you dip too low in deep sleep.
To address your second question, if you’re on a hybrid closed-loop system you might want to increase your sensitivity factor, but if you’re on a pump that doesn’t communicate with a CGM, then lowering the basal rate would be a good idea, and if your lows occur within 2-3 hours after eating, it could be the pre-meal bolus. So timing is important.
Dr Edelman, thank you so much for taking the time to reply! I’m on MDI (Lantus basal) at the moment. Interestingly, I had my first low bloody sugar after I wrote that comment (must have jinxed myself!). Despite only having had one real low blood sugar so far, my CGM is very “proactive” and is waking me up at all hours with false alarms. Another motivator to get my overnight level a bit higher 🙂 Thanks so much for your insights. It’s very interesting to hear about the pumps and closed-loop systems, and no doubt something that I’ll learn more about in the future. I’m newly diagnosed so trying to learn as much as I can. Will discuss this with my doctor – thank you again!
Oh I should say for anyone reading my comment and becoming increasingly concerned – when I say 4 or 5 I’m taking mmol/l not mg/dl 😅 Thanks again, Dr!
Anytime – if you haven’t yet seen the videos we have on hybrid closed-loop systems, please check them out here (or in our video vault on our website):
https://www.youtube.com/watch?v=cILAWrV8zPA&t=1403s
https://www.youtube.com/watch?v=rt4669nK3hQ&t=953s
Good luck, and let us know if you have any other questions!
I will most certainly check those out! Best wishes 🙂
Can you please do case studies of pump downloads and how to adjust the settings for some difficult cases and different scenarios? Or point me in direction of best resources to make these decisions? Starting a clinical in endo. Ty 🙏🏼
You may want to reach out to Gary Scheiner’s team at Integrated Diabetes:
https://integrateddiabetes.com/
T1D BRITTLE,NEED HELP.WHERE IS THE Help To CONTROL Type 1 BRITTLE Diabetis ??
Hi Raymond,
Dr. Edelman recommended that you take a look at the following videos:
Tips and Tricks for Managing Post Meal Highs
https://www.youtube.com/watch?v=FesZJmeQlKs
The Only Type 1 Lecture You’ll Ever Need
https://www.youtube.com/watch?v=3sp-15o-QcA
New to Type 1 or Haven’t Gotten It Figured Out Yet?
https://www.youtube.com/watch?v=l8R3I2FuI5E
Hope that helps to get you started, and we have lot of other videos in our video vault and on our youtube channel here:
https://www.youtube.com/playlist?list=PLN-L1716i5afHYgqyNQHLftnsbq2eJph1
Interesting I’m newly diagnosed type 1 too with no help, trying to figure it out myself thanks for the links I’ll have a look, I’m lowering my basal more and more and it’s all right but as soon as the gap between meals becomes too big or I have too much exercise I go low
If you still get low when there’s widely spaced meals, then your basal rate it too high. If you’re wearing an insulin pump, make sure you put it in exercise mode at least an hour before you exercise so there’s no insulin on board.
Thank you for your response. I’m getting lower and lower, I’m now on 4 tresiba. They put me on 20 toujeo and then 14 tresiba. I got hypos 24/7. They stopped helping me after 2 months, I’m on my own and went each month down with 2U. How low can you go? Now 4U it looks good, could eat after more than 4 hours without a hypo today. The exercise is a major problem, I don’t have a pump or CGM.I hope with the low basal I can bicycle around without eating before during and after every hour without insuline with this low basal rate. I can’t move around with insuline that goes wrong. I’m very skinny btw bmi 17 I’m 60 years old but use rates for children they suit me best. Every advice for diabetes is for type 2 and obese and i can’t use that.
Thank you for your advice, I’m watching your video’s
You really need to speak to your own doctor. If you are on both Tresiba and Toujeo, that’s two basal insulins. It sounds like you need to cut your insulin dose in half if you’re getting low that much. But please call your healthcare provider today. I am not your doctor and know so little about you, I cannot advise you over the internet.
Thank you i was on toujeo then they switched it to tresiba, i’m fine now. I don’t have a doctor or any support. I’m on my own. I had two visits after I was discharged from a hospital for dka and diagnosed with type 1. I’ll manage, thank you
If you would like, please email Lynne at lynne@tcoyd.org and let her know where you live, and I can see if I know of a good doctor in your area.
Thank you, that’s very kind of you