
- Both type 1 and type 2 diabetes can affect your bone strength and increase your risk for fractures.
- Not everyone with diabetes will experience poor bone health, but certain factors like poor glycemic control, retinopathy, neuropathy, nephropathy, and the length of time you’ve had diabetes can increase your risk.
- Preventing bone loss with diabetes involves a multifaceted approach including nutrition, supplements, lifestyle habits, and exercise.
- Screening for bone health is performed with a bone density scan. Everyone with diabetes should get a bone density screening at age 50 (sooner for some).
- Osteoporosis treatment focuses on slowing bone loss, increasing bone density, and preventing fractures. Treatment options include medications, lifestyle changes, and dietary adjustments.
Reading Time: 4 minutes
Many people are aware that diabetes can affect various parts of the body, such as the eyes, kidneys, and nerves. However, not everyone knows that diabetes can also have a significant impact on bone health. This lesser-known complication of diabetes, often referred to as “diabetic osteopathy,” is an important consideration for those living with diabetes.
Keep reading to learn more about diabetes and osteoporosis and what steps you can take to improve your bone health.
How Does Diabetes Affect Bone Health?

Similar to how high blood sugar levels and vascular disease contribute to other diabetic complications, these factors also play a role in affecting bone strength and increasing the risk of fractures.
The chronic inflammation associated with obesity, combined with the effects of hyperglycemia, can weaken bones and lead to a higher risk of fractures and poor fracture healing.
Can Bone Loss Happen in Both Type 1 and Type 2 Diabetes?
Yes, type 1 and type 2 diabetes can each affect bone health, though the mechanisms and presentations differ between the two.
Bone Loss with Type 1 Diabetes
People with type 1 diabetes tend to have lower bone density, leading to a higher risk of osteoporosis and fractures with aging.
Bone Loss with Type 2 Diabetes
Historically, it was believed that individuals with type 2 diabetes, who often have higher body weights, were at a lower risk for osteoporosis and fractures. This belief was based on the idea that increased body weight provides a mechanical load on bones, potentially strengthening them.
However, research has shown that despite a trend toward higher body weight, people with type 2 diabetes actually have a higher risk for bone fracture compared to those without diabetes.
What Is Osteoporosis?
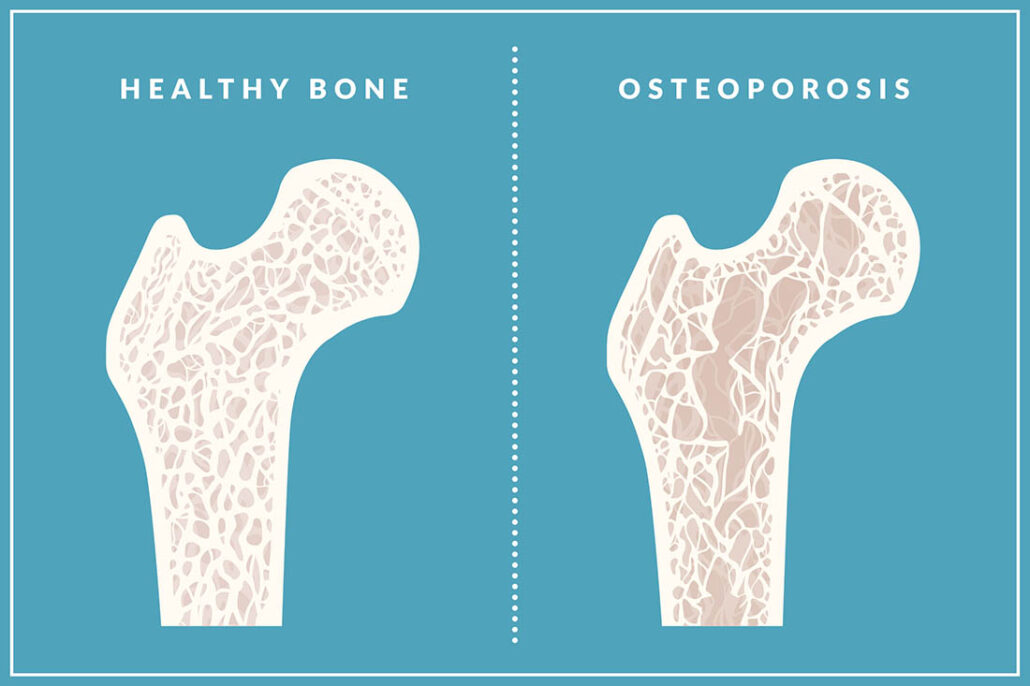
Osteoporosis is a condition characterized by low bone mass and deterioration of bone tissue, leading to weak, brittle bones that are more prone to fractures. It develops when bone loss occurs faster than bone formation, making bones fragile and increasing the risk of breaks, especially in the hip, spine, and wrist.
Is Everyone with Diabetes at Increased Risk for Bone Loss?
Not everyone with diabetes will experience poor bone health, but certain factors can increase the risk for this diabetic complication.
Risk factors include:
Longer Duration of Diabetes
The longer someone has diabetes, the greater the risk for bone complications.
Insulin Use
People with type 2 diabetes on insulin therapy may have an increased risk of fractures. This may be related to falls resulting from hypoglycemia.
Microvascular Complications
Complications of diabetes like retinopathy (eye disease), nephropathy (kidney disease), and neuropathy (nerve damage) are linked to a higher risk of fractures.
Poor Glycemic Control
Consistently high blood sugar levels can further weaken bones.
How to Prevent Bone Loss and Fractures
Preventing bone loss and fractures – especially for those with diabetes – involves a multifaceted approach.
Nutrition

- Calcium: Recommended calcium for adults 19-50 is at least 1,000 mg daily, with older adults requiring around 1,200 mg daily. This can be achieved through a combination of diet and supplements. Dairy products and calcium-fortified foods, such as certain plant-based milks, are excellent sources of calcium.
- Vitamin D: Vitamin D is crucial for calcium absorption. It can be obtained through sunlight exposure, foods like mushrooms and egg yolks, and fortified products. While taking vitamin D alone may not significantly reduce fracture risk, combining it with calcium is beneficial for bone health. The recommended daily amount of vitamin D is 600 IU for people ages 1 to 70 years, and 800 IU for people over 70 years.
- Protein: Sufficient protein intake is essential for preventing muscle loss with aging, a condition known as sarcopenia, which can indirectly affect bone strength.
Individual supplement and protein needs vary, so talk to your doctor about the right amounts for you.
Lifestyle Habits

- Avoid tobacco and excessive alcohol: Both can negatively impact bone health. Smoking causes an imbalance in bone turnover, leading to lower bone mass and increased vulnerability to osteoporosis and fractures. Long-term alcohol consumption interferes with bone growth, resulting in decreased bone density.
- Maintain a healthy weight: Being underweight can increase the risk of fractures.
Exercise
Exercise is beneficial for people with diabetes because it helps improve blood sugar control, enhances overall health, and reduces the risk of complications. Here are a few ways it can also impact bone health:
- Resistance or strength training: Engaging in strength training at least twice a week helps build muscle and strengthens bones. Exercises like squats, lunges, and shoulder presses are examples of resistance training exercises.
- Impact exercises: Activities that involve impact, such as step-ups and jumping jacks, stimulate bone formation by applying mechanical force to the bones.
- Balance training: Performing regular balance exercises, such as Tai Chi or simply standing on one foot, are effective in preventing falls, a major cause of fractures in older adults.
Always speak with your doctor before starting a new exercise program.
Menopause Considerations
Women nearing menopause should consult with a healthcare provider experienced in menopause care. Menopause hormone therapy can effectively prevent bone loss and reduce fracture risk, but the decision should be weighed against potential risks.
How Is Osteoporosis in People with Diabetes Diagnosed?

When it comes to diabetes and osteoporosis, anyone with diabetes should get a bone density screening at age 50. It’s generally recommended that people without diabetes (and without certain medical conditions) get a bone density screening at age 65.
Screening for bone health is performed with a bone density scan (DXA) scan. This is a low-radiation test that measures bone density in the spine and hip. DXA results are expressed as a “T-score”. Lower T-scores indicate lower bone density and higher fracture risk.
A T-score of -2.5 or lower is used to diagnose osteoporosis.
For those with type 2 diabetes, bone density measurements may underestimate fracture risk, so a slightly higher threshold (T-score of -2.0 instead of -2.5) is used for diagnosing osteoporosis.
Individuals who experience a low trauma fracture of the hip or spine are automatically diagnosed with osteoporosis, regardless of the T-score.
What Are the Treatments for Osteoporosis?
Osteoporosis treatment focuses on slowing bone loss, increasing bone density, and preventing fractures. Treatment options include medications, lifestyle changes, and dietary adjustments.
If you are diagnosed with osteoporosis, several effective treatment options are available, including oral medications, IV infusions, and injections. These treatments can significantly reduce fracture risk and improve bone strength.
Some anti-osteoporosis medications can affect carbohydrate metabolism, so managing diabetes alongside osteoporosis may require a more tailored approach from your doctor.
Diabetes and Osteoporosis: The Takeaway
Make no bones about it, taking care of your skeleton is an important part of taking control of your diabetes. In order to be as strong and healthy for as long as you can be, paying attention to your bone health is essential.
By understanding the risks, engaging in preventive measures, and seeking appropriate screening and treatment when necessary, you can maintain strong bones and reduce the likelihood of fractures.
Regular check-ups with your doctor and staying informed about your bone health are key steps in managing this often overlooked aspect of diabetes care.
Your bones need your support – you can’t leave home without ‘em!
Be sure to check out our podcast on diabetes and bone density, as well as our resource library for more tips on living well with diabetes.
Additional Resources:

At 53yrs, I’m postmenopausal and have had type 1 for about 13 years. The podcast inspired me to have a DXA scan, which showed osteopenia. I’m happy to know so that I can take action now – I’ve just started hrt and hope that it may slow further bone loss. All of your podcasts have been super informative. I love that you both have personal and medical experience with Type 1. It’s easier to laugh at the challenges when I know you’ve been there too.
Thank you so much for your comment…really appreciate it!