
The A1c has been around for a long time and is supposed to give people with diabetes and their healthcare professionals an idea of what the average glucose value has been over the prior two to three months.
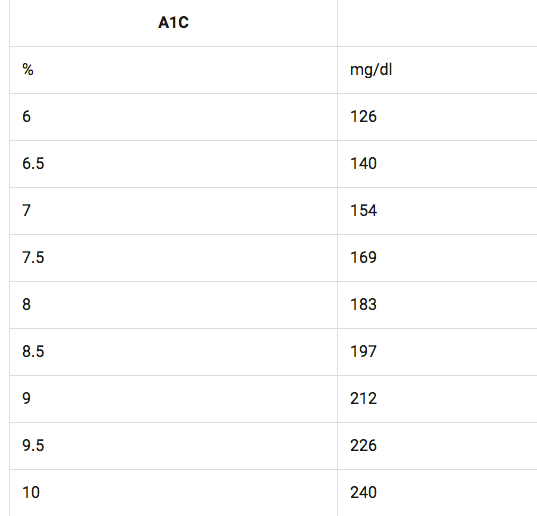
For example, an A1c of 7% would equate to an average glucose value of 154mg/dl (see table).
The A1c has been an important test since most folks with diabetes cannot prick their fingers every five minutes, 24 hours a day for three months and then just take the average. They would need a blood transfusion on a weekly basis! I will come back to the role of CGM (or continuous glucose monitoring) a little later.
Why Does the A1c Suck?
A1c accuracy isn’t reliable because it does not tell you anything about the fluctuations in your glucose values throughout the day and night, which is extremely important. If your A1c is high, you know your glucose is on the higher side in general, but you still can have serious, unrecognized low values and would never know it. On the other hand, if your A1c is low, you are probably having a lot of lows but with no clue what time of day, and be fooled since you are “at goal” with an A1c below 7%.
In addition, there are many situations where the A1c is not accurate. First of all, the laboratory methods of each hospital or clinic may be faulty, and this is not an uncommon situation. At UCSD where I work, the laboratory had an issue measuring the A1c falsely high by 1 or more percentage points. This really upset my patients as the A1c test did not match their glucose values. Having a falsely high A1c is like being falsely accused of a crime and once in your medical records, it is impossible to take out. You will then be labeled as a “bad diabetic” by caregivers who look over your results.
You may also get spurious results if you are African American or pregnant (or both). If you are anemic (low blood count) from kidney disease or other chronic illnesses, the A1c may be artificially low. Sometimes we just cannot figure out why the A1c does not match home or continuous glucose monitoring results.
On the other hand, the availability of CGM has opened our eyes to the inaccuracies of the A1c test, but also has given us new glycemic indices or ways to measure how our diabetes management is doing. A typical CGM will give you and your HCP the average glucose value and SD (standard deviation or degree of bounce) over the past three months, made up of 25,920 values if you wear your CGM 24/7.
You can get an extremely accurate estimate of your A1c simply by plugging it into this formula: eA1c = (average glucose + 46.7) divided by 28.7, or you can also go online and plug your average glucose value into this eA1c calculator.
This is my famous quote so pay attention:
“The most accurate way to measure the average glucose over the past three months is to measure the average glucose over the past three months!”
And now we can do it with CGM devices.
What Is Time in Range?
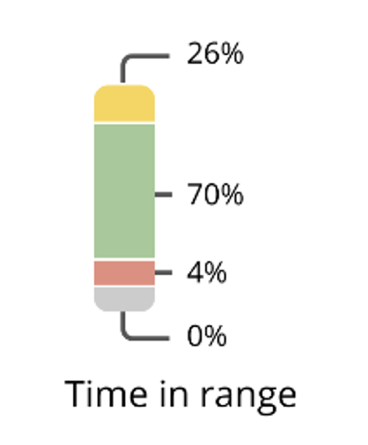
The CGM downloads now all give a measurement called TIR or Time in Range. It is defined as the time spent between 70 and 180 mg/dL. It simply is a measurement of the ups and downs over a period of time. TIR really says it all as it typically gives the percentage of time above 180 and below 70 (see diagram – the yellow section is time spent above 180 mg/dL, the green is between 70 and 180, the red is below 70 and the gray is below 55.) It also relates to how much you are fluctuating throughout the day and night. A good TIR is 70%, and folks on the artificial pancreas systems are getting in the 90% range!
When I see patients in my diabetes clinic, I look immediately at their average glucose, standard deviation and TIR. Not everyone has a CGM and not everyone needs one, but every type 1 should have one. If you have type 2, are NOT on insulin, have a great A1c and are not taking any medications that cause hypoglycemia, you probably do not need a CGM and the A1c will be important. It is a new era of looking at time in range, which is so important to us folks living with diabetes compared to the A1c.
Additional Resources:
5 Ways to Turn Your A1c Into Action
Which Is Better…a Lab A1c Test or the Estimated A1c (GMI) from a CGM?
How to Improve Your Time in Range Solely by Adjusting Your Alerts and Alarms!
The Benefits of CGM and Time in Range for People with Type 2 Diabetes
How Does Time in Range Affect Quality of Life?
Facebook Live: Everything You Need to Know about CGMs


I agree the A1C does not show your lows and highs, I don’t like it when my Endo says, you are doing great because your A1C is 5.7 and I tell her that she should look at the CGM report which would actually tell her that I had lots of lows and some highs and we should discuss how to minimize that. It’s wrong for doctors to look just at the A1C, but most of them do.
We agree Renate – especially when we have so much more information available at our fingertips now. Thanks for your comment!
There is a better way. Look up Glycated Albumin.
What about when your A1C is 10. They change your insulin to a combined dose and it goes up to 12. And need to get it to 8 before they’ll do a surgical procedure. I have to tell nurse need to adjust meds.. Waiting on 1-2 wks of meter readings to give her.
Agreed. And I have to get my test kit and pump sneaked in to hospital to get my own bg in a range to be released. Sliding scale has never worked for me.
Get a pump and cgms and watch the a1c number fall dramatically if you learn Sugar Surfing techniques. Modern equipment is so vital.
What is the target for TIR (time in range)? And what is the range that folks should use? Our studies have shown that a home test for HbA1c is very useful for indicating the effectiveness of a change in therapy and we have seen the A1c deop in as little as 2 weeks from a therapy change leading to an improvement in glycemic control. For everyone who does not have a CGM, I urge that test their A1c at home and test whenever a change in therapy is made. Now is not the time to throw out the HbA1c test.
Hello John,
Not throwing out the A1c at all. TIR is defined between 70 and 180 as I said in the article and video (better get back on your ADHD meds! 🙂
TIR is more important on a day to day basis for people with type 1 diabetes since our glucose values bounce around a lot.
Thanks for your comment John.
I am an nurse practitioner student and am grateful for the information that you have provided. I used to work for a family practice MD that focused on the A1C almost exclusively with his type 2 patients. The patients were frustrated that their glucose monitoring was not regularly evaluated. I have found many pearls in your updates since attending a TCOYD conference with my friend with type 2 DM. Thank you.
Thank You Janet! 🙂
I’m a T1D and have been looking at the SD in my BG readings ever since I first started using a CGM. Invaluable information but very tough to get it down from 40’s to 20’s (my goal). One thing that would help immensely is an algorithm for determining how much ingestion of fats and proteins are affecting my BG. I try not to eat too many carbs but bolusing purely on carb count flat out doesn’t work. I think that should be an area of study in the research community. I don’t know about the rest of you but it would sure help me. Thanks TCOYD team for all you do.
Thank you for your thoughts, Randall!
It would be great to have an understanding of how to bolus for higher fat content foods. I bolus almost exclusively according to how many grams of carbs I think I’m ingesting and you’re right it’s not enough information to keep my post meal sugars in range !
Hi Cia,
There are no set rules or perfect formulas. You could give a square wave bolus if on a pump, and having a CGM is also helpful to see when the directional arrows turn upward, and then a small bolus. It is really trial and error, or the WAG method…(Wild _ss guess)!
Learn to Sugar Surf with Dr Stephen Ponder. Then with Auto Mode pump, you can learn to allow for protein and fat! My dh had a late supper of scrambled eggs, broccoli and 1.5 slices of ham and 1 slice of bread and 1 c. of milk. I expected his bg to run high all night. But it stayed at about 6.5 according to the cgms with one small excursion at 1:30 am where I gave 1 unit of insulin. When I finally tested this morning, his bg was 7.0 and his units for first 11.5 hours of the day were about 19.5 units of insulin. So the AM feature of the pump did its job. Normally his insulin usage would be about 1 unit an hour not nearly 2 and I didn’t have to fight all night to keep the bg in range. That’s what we want, isn’t it? Big kiss to AM.
When the A1c came into being it was the way that those who would cheat on a fasting blood sugar would get caught in the reality of what was happening with their daily control for 2 to 3 months, but yes – it does not show what is happening with highs and lows during the 24 hour day. Fortunately, my primary care giver does ask and knows that the A1c is not the answer, but I cannot get approved for a CGM. We have tried and though I have been told Medicare will now cover, I apparently don’t meet DexComs qualifications. It is frustrating to say the least. I have been Type 1 since March 1956 when I was 4 and 1/2 years old. I still take multiple shots each day and do not use a pump as that is what I prefer. Any suggestions as to another route to take to get a CGM would be appreciated.
Marilyn,
If you are on Medicare you should absolutely be able to get a Dexcom G5, and soon the G6. You should email Danielle Hart at Dexcom to find out. Her email address is: danielle.hart@dexcom.com and you can copy me in your email to her. My email is: Steve@tcoyd.org
Thank you for this information. What I would like to know is are you or others also looking at circadian rhythms and rx delivery and/or glucose testing. I have always been an early riser and am in bed by ten. Would CGM reflect my situation versus a night owl?
Absolutely it would. When you look at the 24-hour glucose profile, you should be able to look at the time of day and see how you are doing on a day to day basis.
Absolutely it would. When you look at the 24-hour glucose profile, you should be able to look at the time of day and see how you are doing on a day-to-day basis.
Why is TIR calculated based on up to 180? If I am always 150-180, that is too high, but could theoretically get to 100% TIR with high BG all the time.
FTR, I try really hard to get to non-diabetic BG levels and still struggle. I have a CGM already, but would much rather see better BG management methods than just changes to metrics. I woud love to just be at 100 steady all day and all night. 180? Not so much.
The 70 to 180 is meant to get pre and post meal ideal ranges for most people.
I agree with that comment. I think 180 is too high. I go way up in the morning without even eating and my 670g is not giving me enough basal at this time. If I am not in automode and Bolus, by 10:00 I am great. Without the Bolus I am high till 1:00 or so… in the 200’s and I am not eating a lot of carbs.
It surprises me that you can be within 30 points all the time. I’m T2 on insulins and while I’m under 6 A1c and TiR of 98%, I see commonly see individual readings from 70-160 and beyond.
As a non-professional, I’d say that staying 150-180 is great, you aren’t extending into any of the really dangerous numbers. But staying on the high end tends to suggest its time to add a little insulin or change the overall regimen
My insurance doesn’t cover a CGM, maybe I can get one and supplies cheaper outside of the US? Everything else is like that
Hi Wayne,
We’re not privy to all of the pricing on each CGM, but it’s certainly worth a try to search for any way to get these supplies cheaper. We hear you!
Insulin and other meds are a lot cheaper, but pumps and cgms are not in Canada compared with the U.S.
Hi. Great article to learn more about TIR. I have had T1 for 31 years and never had an A1C over 7.2, but had large swings on most days. My A1C for the last 10 years has been 6.2 which I strive hard to achieve since my sister who is also T1D had a pancreas transplant. Her transplant scared me. Now I am starting to have tingling in my legs which is disappointing since on paper I looked awesome for years! But, TIR is more important I am now learning. I started the Medtronic 670G recently and really struggling. I am trying to cope with the pump thinking 150-180 is a good blood sugar, bc I want to be 100-120. Now I am striving for a new goal of TIR of 78-82%. It’s a daily struggle and a new way of thinking.
Hi Carolyn,
Congratulations on doing so well with your diabetes over the years! Having a really good A1c is always extremely important in the long term, and it has served you well. Early diabetic neuropathy (I’m not sure if that’s what you have) can be treated, and thankfully is not a serious issue right now for you. The 670G I know takes a lot of effort to stay in auto mode, but hang in there and keep your eyes open for newer advances in pump CGM combinations.
I’ve had T1 diabetes since 1964 and about 15 years ago I developed neuropathy In my feet that didn’t bother me because it was like wearing toe socks or something. ( just numbness.)
But then it became painful and I was having a hard time walking and was perpetually exhausted. Someone suggested I try the alkaline diet popularized by Robert O. Young. I am not kidding you – within four days of radically changing my diet, my energy surged and my feet lost all numbness. But it was at a price.
I had to give up wine which I loved, coffee, and all the foods that produce acid in the blood. It’s been worth it and I’ve stayed close to that diet ever since. If I deviate and have a half glass of wine my toes go numb for a day or so, but they always lose the numbness again if I get back in line .
Thank you for sharing, Cia, and we’re glad you found something that works well for you.
How do I find the time in range? I’m new to the cgm and I have the Tslim pump.
Hi Sally,
It would be best for you to call the 800 number at Tandem (877-801-6901) and they can walk you through downloading the app which will then have TIR on its reports.
It is interesting that you mention the A1C not being trustworthy. I have one at 6.4, but I get frequent meal spikes in the 200s and above. I am a type 2 and do use long acting, fast acting and oral medications. My TIR is good, I think in the high 70s, but my Endocrinologist says my deviation needs work (which I wasn’t aware of before). So despite 12 years of diabetes and A1Cs under 7, I still have complications starting now, but only in the past year to coincide with the spikes.
So if the complications are tied to spikes and not A1C, shouldn’t surgeons be alerted to look at TIRs and deviations before surgery? Surgery usually interrupts our activity portion of control and the trauma additionally increases blood sugars. Wouldn’t it be prudent for them to realize that A1C can dramatically change with surgery and prompt them to look for other methods of clearing diabetics for surgery?
Hi Helena,
The A1c is still important, and congrats on yours being good! My point was that in addition to A1c, the daily swings (TIR) are also important. 70% is good. And…surgeons do not know much about diabetes in general, and surgery does mess up our blood glucose levels but for short periods of time. Remember that short time periods of poor control are not harmful. Thank you for your question!
Thank you Doctor. Well presented and very concise. As I have lived longer with T2 diabetes for 22 years and have been studying for awareness talks, I have been focusing basically with the point of glycemic triggers and spikes and time in range. I feel that I am on the right path. Now, if my insurance would approve the Libre, life would be so much better. I hope we have a chance to cross paths.
Thanks for your comment Michael!
I totally agree, that the TIR is just or if not more important than the A1c. A good meter will tell you what your 14 day , 30 day and 90 day averages are.
The problem is diabetics do not like testing, especially the type 2’s.
The CGM makes me read low and high and I count my carbs. Please give me some pointers
Hi Lori,
Dr. Edelman devoted an entire chapter of his book to continuous glucose monitoring (chapter 10) if you would like more information, but you should also speak with your endocrinologist (or healthcare provider) who knows you and your health history and can answer questions specific to your situation.
Enlightening article. Helped me understand why my endocrinologist was pleased with TIR and not too concerned of minor increase in my A1c.
My father has type 2 for 20 yrs, not on insulin just same medications for 10years, his A1C is 6.9 and has been good for years. He recently got diagnosed with diabetic retinopathy and just had surgery. Should his doctor do more to test his levels besides the A1C test every 6months since this has happened or is diabetic retinopathy just a cause from having diabetes for so many years. Is his diabetes really under control because his A1C has been good for so long?
Yes, an A1c around 7 is excellent, and since they caught him early, he will do well and avoid serious vision loss. Stay in close contact with his eye doctor.
Loved this article & would love some extra advice, if you have time! I have a huge family history of diabetes & I just looked at my charts. It seems my A1c levels grew from 4.6% to 5.0% from July to December. Should I keep testing my A1C levels, just in case? I am also worried about adrenal fatigue since I have a High DEHA of 465 ug/dL & low vitamin D. I just got a referral to an endo, but any advice or connection between everything would still be appreciated!
Hi Kayla,
Thank you for your question and for sure you should follow your A1c every 3 to 6 months. As far as adrenal issues go…that is much more complicated so I’m glad you are seeing an endo. You seem like you are staying on top of things so big kudos on that!
I was recently diagnosed with type-2 diabetes. My A1c was initially 6.5. When I did the second A1c test to confirm it, only four days later, it was 5.9. I ate very healthily for four days before taking the test again. My doctor prescribed me the lowest dose of metformin. My question is, if the A1c is an average of the past 3 months, why were my test results so different only four days apart?
GREAT QUESTION! The A1c is a laboratory test and is often inaccurate and not precise. In any case, you are doing well!
lI read they were supposed to have two test results 6.5 or higher to diagnose to begin with
Dear Doctor Edelman
Wonderful post, it makes absolute sense, and what I have thought for a long time, having been a person victim of two situations.
1.
1 A1C discordant test at 8.1% which showed average sugar of 128mg/dl. Note, time of the test 3 months prior all finger blood tests were normal non diabetic range i.e. fasting 80mg/dl 2hr after eat 98mg/dl, random any time after eat 89 or 90mg/dl. 8.1% average should have been in vicinity of 183mg/dl and not 128mg/dl There was a DOUBT on this area.
Here in Spain I did not get the opportunity as I request to have a 2nd test due to inconsistencies between A1C, and real blood finger tests majority all non diabetic range.
Result, I was labelled Diabetic and on record. This is a serious situation, and I cannot reverse this.
since this test my A1C have been 6.4%, 5.8%, 5.6%, 5.4% 5.2%, 5%, 5.2% over one year 4 months, and again, the continued normal non diabetic finger tests continue perfect.
Without doubt, I feel there was a Lab error, i.e. either typographical error the 8.1% should have read 6.1% as average sugars for this value was 126mg/dl, and or there was a lab error generally, as the ratio of the 8.1% with 128mg/dl finger tests, did not seem correct.
2.
Also became victim of where you are in the world depends time of diagnosing, i.e. Australia/Tasmania, the cut off for a1C diabetic is 6.7% or equal to is viewed with 2 tests same as diabetic, v. other countries where cut off i.e. Spain is 6.5% one A1C test only for diagnosing Diabetes.
It was once upon a time not long ago the WHO in their official website, declared that they did not feel that A1C was a reliable marker for Testing, due to variations generally, I believe now they have changed their mind on this policy and allow the A1C to be used, again there is Doubt as to the accuracy of this Test.
I have to say the explanations, and information provided on this blog content was excellent and very very interesting to say the very least.
thank you.
JMD
Thank you for your comments and feedback, Jenny! One thing that doesn’t suck is sangria from Barcelona!
Thanks for this.
Diagnosed with type 2 in May. .. 289 11.6… been pretty strict with diet and exercise.. July my numbers were down to 8%.. I am not on insulin .. started with glipizide and metaformin.. just doing metaformin now. 500mg x2 times daily… I track my A1c 2..3 times a day…. get readings anywhere from low 80s to high 110s.. my question.. are those swings ok.. normal.. .. getting my 3 month check again in September.. hoping for low-mid 6 or lower…..
Hi Mike,
Your goal should be close to 7%. Trying to get lower is not needed and can be dangerous. Good luck!
Hi doctor,
As I understand, A1C test is the percentage of Glucose attached to the red blood cell in 90 days.
Also, as I understand, Glucose attachment to the red blood cell is, a continuous process.
So the question is, test of A1C is for 90 days blood cell or 60 days blood cell or the the blood cell day test was done, which one.
The A1C is an important laboratory parameter that gives doctors and us folks living with diabetes an idea of what our glucose control has been over the past 2 to 3 months. I call the glycosylated hemoglobin (also known as A1C or HgbA1c) the “longterm glucose control factor.” When the glucose level in one’s blood is high for an extended period of time, the excessive glucose molecules stick or bind to many structures in the body, including the red blood cells, which contain an oxygen-carrying substance
called hemoglobin and other proteins. The average life span of red blood cells, which are being produced and cleared from the body continuously, is about 2 to 3 months. When we measure the amount of glucose on the hemoglobin of the red blood cells, for example, it is called the glycosylated hemoglobin, and is indicative of the amount of glucose in the circulation over the past 2 to 3 months.
My question is: my husband is a type 2 diabetic he just got home after spending a month in the hospital where they was always allowing his blood sugars to get up to 400 and giving him the smallest amount of insulin they could give him which was 7 units of Lantus when he was at 400 then the same week he got home after having his blood sugars messed up for a month he did a a1c his previous a1c was 5.7 the one he just had after the hospital stent was 5.2 we are calling it a faulty test but would like to know what you think
The A1c test is really inaccurate. If he had a blood transfusion or was anemic this would make his A1c artificially low. Kidney problems will also do it. I am guessing that was the case. I hate they let people with diabetes run really sweet in the hospital…NOT GOOD!
Was diagnosed with T2D a year ago and was put on Farxiga and metformin. After 2 months was taken off Farxiga. Had lost almost 50 pounds. Then put back on 25 pounds over the next 10 months. Is this normal?
Just had an A1C drawn with 5.8 my number. Is this a good thing? My fbg is usually 93-120. But if my fbs is below 90 I feel bad. What questions should I ask my doctor? Also have thyroid problems (Hashimoto’s and Grave’s disease). Would these diseases have an impact on this?
Your case is complicated. The wide swings in weight is not that normal, and thyroid issues (too high or too low) may be playing a role. Your glucose values are excellent, so congrats. I would ask your doctor about your thyroid status and is it normal. Good luck.
Had kidney surgery a year ago and was given insulin periodically. Have always been told I was pre diabetic with my A1C always at 6.2 with low sugar diet. Having surgery on other kidney since I had growths on both. All biopsys were negative and hope for same on this surgery.
Do I understand that surgery can spike glucose?
Absolutely yes, and make sure to ask them if you’re getting any steroids, which may be perfectly appropriate for your surgery, but just good to know so you can plan for elevated blood sugars.
I’m new at diabetes. Probably had it or some version of it, pre perhaps, for years without knowing. Sugary cereals spiked me to 254 and by lunch I was hypo and shaky and below 70 somewhere according to my readings.
Annual comprehensive metabolic panel test showed morning glucose after fasting since 2014, above 100 and no higher than 131ish. So August 30, 2021, I bought a Contour meter and test supplies and am running my own unscientific testing.
1st week avg. 144
Now Sept 15th 2021, have the average down to 120 with just diet changes.
Calculated my own A1c after 2 weeks of testing, based on 142 avg. And got 6.4 as I remember.
Had an A1c test yesterday Aug. 14th and it came back 5.6 and 114 average mg/dl. If that’s 3 months its not accurate.
My meter is dead on according to the control solution test.
I agree with the doctors article that they are innacurate. Because of so many variables, like blood travel time to testing site and turnover. Supposedly drops in glucose level 5-7,% per hour of travel time are possible. Etc.
I’ll continue sticking my fingers, dont trust the test
My finger stock bloood sugar averages.throughout the day are ALWAYS 90-107. I eat very low carb and am type 2 diabetic (two years) how A1C works…..but what O don’t understand is why the heck it is ALWAYS 6.1 or 6.0 yet no random or fasting or 2 hour blood sugar is EVER above 124. It’s really concerning to me because I spend so much time analyzing my diet macros, and keeping my blood sugars in control (1 metformin 500 mg ER tablet per day) when my A1C (measured at a couple Of different institutions) is consistently higher than my average blood sugars. Very puzzling and I am a clinical lab scientist by trade.
An A1c of 6.0/6.1 is about the range for an average blood sugar of 120. If you want your true A1c, wear a CGM for 90 days and it will give a GMI, which is the most accurate report. Lab methods for A1c can be off by .6-.8%.
I have a CGM from Dexcom. I am type 2 and my glucose was out of control for years. Secondary symptoms such as neuropathy and blured vision were starting to show. With the CGM, diet and timed after meals aerobic exercise I have been able to keep myself in range (70-180) for 88% of the time and with an EAg of 132 and no insulin injections That is the equivalent to 6.1 A1c down from my prior numbers of 9.4 A1c. CGMs are are a miracle of modern medicine and a God sent gift to me.
Wow you are awesome! Congrats on all the positive changes! And yes we agree, CGMs are life savers!
I was just recently diagnosed with Type 2 diabetes. The diagnoses was done via a abnormal 3 hr oral glucose test (308 and 311) at the two and three hour mark despite my fasting bg being fairly consistent at 107 and A1C staying around 5.5 – 5.6. For me sorting thru some of this is just confusing. I do tend to fast more than i eat and was reflected in a diagnostic version of a CGM and caught me going hypoglycemic (which is why the OGTT was ordered in the first place) while sleeping and after eating certain foods (sharp spike in bg then tanks often around 50) I do have to say a CGM is an awesome tool. I do have a question can intermittent fasting or not eating regularly affect the A1C results? I am sure as we try and normalize my diet these numbers will go up. I already see it with my finger sticks.
There’s good news to your results. You do bounce up high after eating simple carbs, so please do not do any more glucose tolerance tests. It shows you that eating well-balanced meals does not cause a spike. The fact that your A1c is good shows that overall, you’re doing really well. Intermittent fasting does not affect your A1c. A1c is the result of the duration and severity of hyperglycemia over the past 2-3 months. In addition, for people who are diagnosed early with type 2, they can get low after eating acute carbohydrates, which is totally normal.
Hi Dr Edelman,
Thank you for your response it is reassuring. I agree that the simple carbs are hard for me as well as the refined carbs.I do suspect that folks “what word am i looking for” make adjustments (by nature) when something doesn’t feel good. Food for me has been a sticking issue. I have avoided over the years the simple carbs but not so much the refined ones again i tend to fast extensively. As i test out food combos i can see it in the data (finger pricks). My A1c still throws me for a loop as i can hang out in the 200 + range hrs after eating a seemingly healthy meal.
I will be seeing a dietitian to help (hopefully) we can get a plan to work on my time in range (TIR) as my Glucose variability and come up with a plan to to use a CGM to get what works for me.
Again,
Thank You!
Sure thing…good luck and stay well!
Apparently, you know nothing about A1c. First of all, it has not been around for a long time. 30-years at most. Prior to this, total glycosylated hemoglobin (a far less specific method) was in use. Second of all, A1c doesn’t have to track daily fluctuations because it gives a 3 month picture of glucose control. This helps clinicians with patient management because, prior to A1c, patients would control their glucose management a week prior to their doctor appointment to get a good reading even though they were not controlling their glucose for the other 11 weeks. Lastly, A1c is important because as it ages it becomes an advanced glycated end product (AGE). AGEs are what cause the complications (sequelle) of diabetes. So, A1c is not only a diagnostic marker, it is the primary cause of the negative effects from the disease. The lower your A1c, the lower your chances of complications.
The A1c is an important test, and used with CGM metrics, it’s even stronger. Thank you for your comment – I appreciate it and learned something from your message.