
Though I don’t have diabetes, I do have obstructive sleep apnea (OSA) which was detected by my lovely wife over 15 years ago. I want to share some of my personal experiences with this diagnosis in hopes it might help others who are not aware they might have the condition. I will also briefly address the current understanding of sleep apnea in people with diabetes.
My Diagnosis:
My wife had complained about my loud snoring for years, but I never associated it with how fatigued and sleepy I felt, especially in the afternoon. I would often struggle to keep my eyes open when charting on my patients at the end of the day, or when reading medical journal articles. I just wrote it off as being due to working long hours and pushing myself too hard. I had become more aware of sleep apnea and the telltale symptoms after we did a research study with some of our patients with type 2 diabetes. In this study conducted by Dr. Dan Einhorn, 35 % of our patients with type 2 diabetes we tested had sleep apnea (49% of men and 19% of women tested had the disorder). I even diagnosed many of my patients with OSA but didn’t recognize the same symptoms in myself. Then after another day of falling asleep into a stack of charts on my desk, I asked my wife, “Have you ever noticed if I stop breathing during the night for short periods?” She said she wasn’t aware of it, but within a few days she came back to me saying she noticed that there were frequent pauses in my breathing during the night. A diagnostic sleep study followed, and I joined the ranks of the millions of people who have been diagnosed with OSA.
OSA Is Common, and Symptoms Include:
- Excessive daytime sleepiness
- Waking with an unrefreshed feeling after sleep
- Having problems with memory and concentration
- Feeling tired
- Experiencing personality changes
- Morning or night headaches
- Heartburn or a sour taste in the mouth at night
- Swelling of the legs
- Getting up during the night to urinate (nocturia)
- Sweating and chest pain while you are sleeping
Symptoms of Sleep Apnea That Others May Notice Include:
- Episodes of not breathing (apnea) during sleep
- Loud snoring (almost all people who have sleep apnea snore, but not all people who snore have sleep apnea)
- Restless tossing and turning during sleep
- Nighttime choking or gasping spells
Risk Factors for OSA Include:
- Excess weight. Fat deposits around your upper airway may obstruct your breathing. However, not everyone who has sleep apnea is overweight. Thin people develop the disorder, too.
- Increased neck circumference. A neck circumference greater than 17 inches (43 centimeters) is associated with an increased risk of obstructive sleep apnea.
- High blood pressure (hypertension). Sleep apnea is more common in people with hypertension.
- A narrowed airway. You may have inherited a naturally narrow throat. Or, your tonsils or adenoids may become enlarged, which can block your airway.
- Being male. Men are twice as likely to have sleep apnea.
- Being older. Sleep apnea occurs two to three times more often in adults older than 65.
- Family history. If you have family members with sleep apnea, you may be at increased risk.
- Use of alcohol, sedatives or tranquilizers. These substances relax the muscles in your throat.
- Smoking. Smokers are three times more likely to have obstructive sleep apnea than are people who’ve never smoked.
- Prolonged sitting. Studies suggest that long periods of daytime sitting can cause fluids to shift from your legs when you recline at night, narrowing airway passages and possibly increasing the risk of obstructive sleep apnea.
Understanding OSA:
Let’s look at this a bit more in-depth, as there are many forms of sleep disturbances:
- Sleep disordered breathing (SDB)
- Sleep apnea (SA), obstructive (OSA) or central
- Chronic voluntary partial sleep deprivation
- Shift work syndrome
- Jet lag syndrome
- Restless leg syndrome
- Insomnia
- Fragmented (fitful) sleep
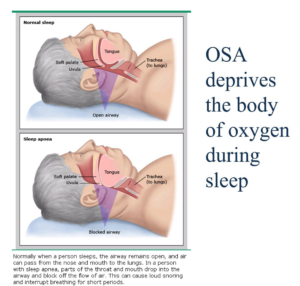
- Menopausal changes
Lack of adequate sleep (regardless of the underlying cause) has both metabolic and behavioral consequences, so improving your sleep habits can have a significant beneficial impact on your health. We will focus here on OSA. The graphic below from UpToDate helps to show visually what is happening in the airway during sleep.
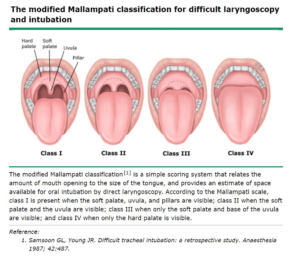
Also, how crowded the airway is will contribute to the problem, and is graded according to the following diagram:
Let’s Define the Terms We Use to Define and Diagnose Sleep Apnea:
- Apnea = stop breathing > 10 seconds
- Hypopnea = 4% desaturation +/arousal (Hypopnea refers to a decrease in breathing, not a complete cessation as in apnea, and this is also associated with a drop in the blood oxygen levels. Arousal refers to a return to a higher level of consciousness from a deeper sleep, though most people do not become fully awake or even aware of the episodes)
- Apnea/Hyponea Index (AHI) = events/hour (adding up the total number of apnea and hyponea episodes that occur in an hour is termed the AHI)
The Severity of the OSA Is Categorized Below by the Corresponding AHI Level:
- AHI < 5 normal (no OSA)
- AHI = 5-15 mild OSA)
- AHI = 15-30 moderate OSA (my AHI was 20, putting me in the moderate range)
- AHI > 31 severe OSA
OSA and Diabetes:
There are significant consequences to untreated OSA including: worsening insulin resistance, increased blood glucose, increased blood lipids, worsening obesity, heart disease, and sudden death. Not to mention accidents and loss of productivity due to sleepiness and fatigue. If you are a snorer and notice that your blood sugar is in poor control, OSA can be a contributing cause, and blood glucose levels may improve with treatment of OSA. Also, poor sleep can lead to behavioral changes, causing poor food choices which may impact weight and diabetes control. This may improve with treatment of OSA (if it’s present).
The following common health conditions can all be worsened by OSA: obesity, diabetes, congestive heart failure, depression, stroke and high blood pressure.
Diagnosing OSA:
Previously, the diagnosis of OSA required you to spend the night away from home in a sleep lab, but now convenient sleep studies can be done in the comfort of your own home. One example is the NOVASOM system shown below:
- Virtually attended portable monitoring system
- Bedside unit uses voice prompts to guide set-up
- Sensors capture five measures (airflow, breathing efforts, blood oxygen, heart activity, snoring)
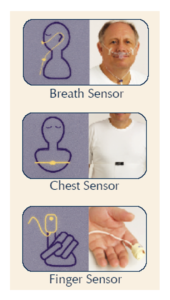
The device is delivered by mail to your home, and returned by mail to the company once you have completed your home study.
What Are the Treatments for OSA?
- Weight loss (sleep apnea will often improve with modest weight loss)
- CPAP (Continuous Positive Airway Pressure) device
- Oral appliances: reposition lower jaw, etc. (for mild to moderate OSA)
- Repositioning: from back to side-sleeping
- Surgery (multiple strategies to increase the size of the airway)
Below Are Pictures of Modern CPAP Devices:


Home bedside unit with humidifier tank Travel CPAP (smaller than an iPhone)
Benefits of Treatment of OSA:
- Heart health: One month of CPAP improves daytime blood pressure, heart rate and left ventricular function
- Stroke and CHF: With CPAP treatment, stroke risk is reduced 35% and CHF is reduced 20%
- Diabetes: After-meal blood glucose levels can be reduced with compliant CPAP therapy, and effective OSA therapy has also been associated with a 10mm Hg fall in blood pressure
A Word about CPAP:
CPAP involves wearing a face mask which may consist of a nasal pillow or a larger mask that covers both nose and mouth. The mask is attached to tubing which is connected to a small beside device about the size of a clock radio. The newer devices are exceptionally quiet, and if you have a sleeping partner your absence of snoring will be most welcome. Even smaller travel devices take up less room in your carry on bag than most small toiletry/shaving kits.
After treatment with a CPAP machine, my symptoms have dramatically improved. No longer do I struggle to stay awake at work, and I feel more energetic. My wife is also sleeping much better without my loud snoring. I do have to admit it did take me almost six months to get used to wearing the CPAP mask at night, but I’m glad I stuck with it as I have such an improved quality of life. Working with a good sleep specialist can help you find the right equipment. It may take several attempts, so don’t be discouraged if the first few tries are unsuccessful.
In Summary
Finally, if you or someone you love is experiencing the symptoms of sleep apnea, a simple conversation with your doctor can initiate an appropriate evaluation to determine if there is a problem. Appropriate sleep therapy may not only improve your symptoms, but it can dramatically improve your overall health including blood sugars, blood pressure and risk for heart disease.


Trying to reach you Chris. Really need a referral. I can explain more. I’m a former patient and I trust your expertise.