- For a cure for diabetes to be successful, we need three things to happen. We need enough islet cells for everyone living with the condition, and we need a solution that doesn’t require immunosuppressants. We also need transplanted islet cells to be durable and last over time.
- It’s now possible to make islet cells in a laboratory for everyone in the world who has type 1 diabetes, so now we need to address the problems of immunosuppression and durability.
- Researchers are working on different ways to protect the beta cells from attack, with varying levels of success. Vertex Pharmaceuticals, Novo Nordisk, and Sana Biotechnology are three companies with promising islet cell transplant therapies.
- Islet cell transplant therapies work, and we believe we’ll see a functional cure for diabetes by 2030.
Reading Time: 7 minutes
People have been saying for years that a cure for diabetes is right around the corner. Well, we’ve been waiting to turn that corner for decades (and who are these “people” setting the time frames, anyway? No one knows). We’re still anxiously awaiting a cure, but we’re truly closer now than we’ve ever been.
Before we delve into the latest research, let’s first explain what we need in a cure and why.
What Causes Type 1 Diabetes?
Type 1 diabetes is a condition that occurs when the body’s immune system attacks and destroys insulin-producing beta cells that reside in islet cells of the pancreas.
Why does this happen? That’s the million-dollar question – scientists are still trying to figure it out. When beta cells fail, too much sugar builds up in the blood, and people need to take insulin daily to survive.
3 Things We Need to Cure Type 1 Diabetes
Three important things need to happen for a cure for diabetes to be successful:
- We need enough islet cells for everyone on the planet living with type 1 diabetes
- We need a way to give the cells back to patients that doesn’t require immunosuppressant medications
- We need to make sure transplanted islet cells will be durable over time
Solving Problem # 1: Using Stem Cells to Make Islet Cells
Stem cell therapy for type 1 diabetes has evolved significantly in the last decade, moving from cadaver-sourced cells to lab-manufactured stem cells.
Initially, researchers relied on islet cells from deceased organ donors. As you can imagine, this method had huge limitations due to the scarcity of donors and the need for lifelong immunosuppression.
Thanks to years of stem cell research in type 1 diabetes, it’s now possible to make islet cells from stem cells in a laboratory for literally everyone in the world who has type 1 diabetes (Steve and Jeremy first!).
What Are Stem Cells and How Does Stem Cell Therapy Work?
Stem cells are cells in the body that have two pretty incredible abilities.
First, they can make copies of themselves, allowing them to replicate indefinitely.
Second, they can transform into various cell types, such as blood cells, brain cells, and yes, beta cells. They offer promising possibilities for treating diseases like diabetes by regenerating damaged tissues.
What Are Islet Cells?
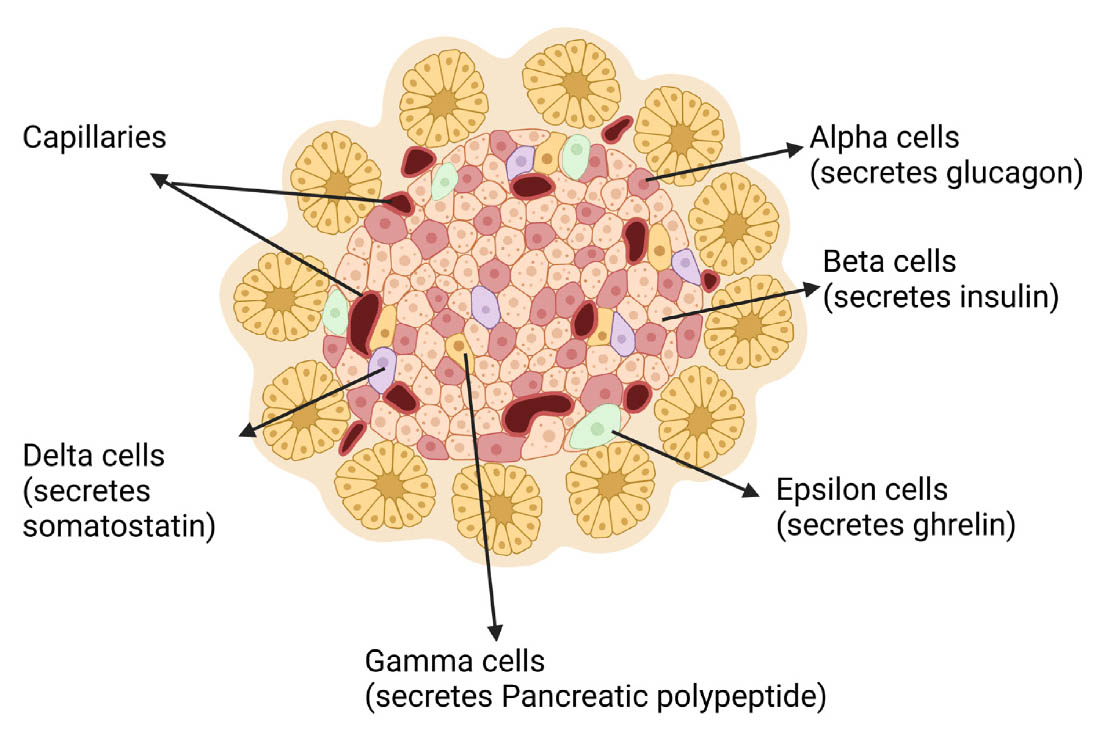
Islet cells are in the pancreas and play a crucial role in regulating blood sugar levels. Islets contain several types of cells, each producing different hormones. Beta cells are primarily responsible for producing and secreting insulin and amylin to help regulate blood glucose levels. Alpha cells produce glucagon to raise glucose levels when low.
What Is an Islet Cell Transplant?
Lab-grown beta cells are engineered to function like natural pancreatic beta cells, capable of sensing blood sugar levels and releasing insulin. Manufactured beta cells are transplanted into a patient’s body (typically into the liver) where they can survive and begin producing insulin and the other beta cell hormones.
Do Islet Cell Transplants Work?
Yes, islet cell transplants do work! The majority of patients in studies who have had islet cell transplants don’t require insulin and are essentially cured, though they are on immunosuppressants for life.
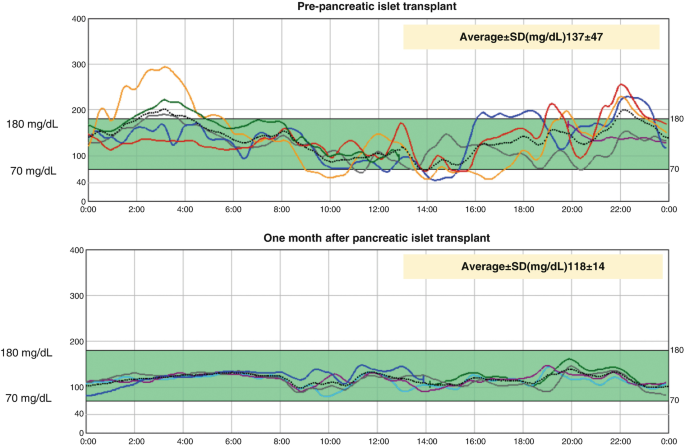
The first image in the chart below shows CGM data from a patient before their islet cell transplant. The second image shows CGM data one month after their islet cell transplant. Pretty amazing!
Addressing Problem # 2: Immunosuppressants
Now that we’ve fixed the islet cell issue, we need to address the problem of immunosuppressants. No one wants to be on immunosuppressants for life. Importantly, the amount of immunosuppressants needed is less than what is required for a whole organ transplant, such as a kidney.
Researchers are working very hard on different ways to protect transplanted beta cells from attack, with varying levels of success.
Addressing Problem # 3: Islet Cell Durability
We also need to make sure that once we put new cells into the body, they’ll last. Several approaches are being explored to enhance the longevity and effectiveness of transplanted cells.
At the most recent EASD conference (European Association for the Study of Diabetes) in September 2024, it was announced that four patients with 12+ months of follow-up after receiving the islet cell replacement therapy VX-880 from Vertex Pharmaceuticals had sustained insulin independence. Of the four, one patient had more than 24 months of insulin independence, as reported by Vertex.
So How Close Are We to a Cure for Diabetes?
Once we figure out how to solve the immunosuppressant and durability issues, we’ll essentially have a functional cure for type 1 diabetes. We believe a reasonable time frame for that to happen is before 2030.
Many companies and researchers around the world are trying different approaches to stem cell therapy, encapsulation, and cell modification. Vertex Pharmaceuticals, Novo Nordisk, and Sana Biotechnology are three companies leading the way.
Vertex Pharmaceuticals

Vertex Pharmaceuticals is a biotech company working on two stem cell-derived therapies:
1. VX-880: A stem-cell-derived islet cell therapy that involves transplanting lab-grown insulin-producing beta cells into patients in the liver. It does require immunosuppression to prevent rejection.
VX-880 Clinical Trial Progress:
At the ADA’s Scientific Sessions in June of 2024, Vertex presented data from its Phase 1/2 clinical trial. Twelve patients received a full dose of VX-880 through a single infusion. By Day 90, all showed successful islet cell engraftment and glucose-responsive insulin production.
At their latest follow-up, all patients had A1c levels below 7.0% and maintained over 70% time-in-range. Impressively, 11 of the 12 patients reduced or eliminated their need for insulin injections. The treatment was generally well tolerated, with no serious adverse events related to VX-880 reported. Two patient deaths occurred during the study, but it was determined that they were unrelated to the treatment.
In November 2024, Vertex announced the expansion of the VX-880 trial into a Phase 1/2/3 pivotal study, aiming to enroll approximately 50 people. Vertex anticipates completing enrollment and dosing for this pivotal study in 2025.
2. VX-264: An encapsulated version of islet cell therapy that uses a protective device to guard implanted beta cells from the immune system, with the goal of eliminating the need for immunosuppressants.
VX-264 Clinical Trial Progress:
The clinical trial for VX-264 is a global, multi-part, Phase 1/2 study. Vertex completed Part A of the study, with patients receiving a low dose with a stagger period between dosing.
Part B of the Phase 1/2 study is enrolling and dosing patients. In Part B, patients receive the full target dose with a stagger period between patients, and in Part C, patients will receive the full target dose with no stagger. Vertex hopes to share initial data from this study in 2025.
Novo Nordisk

Novo Nordisk is a pharmaceutical company with a long history in diabetes management and care. They make several types of insulin and GLP-1 therapies like Ozempic. In recent years, they’ve been collaborating with academic institutions and biotech firms to research stem cell-based treatments for type 1 diabetes.
Their key initiatives include:
- Stem cell-derived islet transplants
- Encapsulation technology
Clinical Trial Progress:
Novo Nordisk is conducting early-stage clinical trials to assess the safety and efficacy of their stem cell-derived therapies.
The big news here is that a long-standing diabetes company like Novo Nordisk is getting involved in this space. It shows the high interest of pharmaceutical companies to deliver an islet cell product that can be used by the masses.
Sana Biotechnology

Sana is much smaller than Vertex and Novo Nordisk, but they found a way to modify cells so immunosuppressants aren’t required.
Their two key technologies include:
- Stem cell-derived beta cells designed to restore insulin production
- Immune evasion technology
Sana’s hypoimmune platform is designed to cloak transplanted beta cells, making them invisible to the immune system. This allows them to evade immune detection without immunosuppression.
Clinical Trial Progress:
In a first in-human study, Sana successfully transplanted engineered pancreatic islet cells into a T1D patient without immunosuppressive drugs. The transplanted cells evaded immune rejection and produced insulin. This was done in only one patient and data so far is only from four weeks after the transplant, so we will be watching closely to see if the effects last and can be replicated in more people.
How to Participate in Type 1 Diabetes Clinical Trials
To find clinical trials in the United States, visit clinicaltrials.gov and search for type 1 diabetes, or explore recruiting trials on the Breakthrough T1D website.
If you’re interested in applying for one of the trials from Vertex, they are looking for people with type 1 diabetes who have severe hypoglycemia unawareness and significant hypoglycemic episodes for their VX-880 trial. You can learn more at 880.t1dstudy.com.
Novo Nordisk has information regarding their studies on the clinical trials page on their website.
Cure for Diabetes: Key Takeaways
The bottom line is that islet cell transplants for type 1 diabetes work! Many people who have received these transplants have come off insulin and are essentially cured.
We have solved the problem of making cells with the development of stem cell technologies. Now, the major hurdle is immunosuppression. We are optimistic that one of these approaches (either encapsulating the cells or genetically modifying them) will be realized in the next decade.
When that happens (not if!), we truly will have a cure for everyone in the world with type 1 diabetes. We know you have all been told there will be a cure for diabetes in 10-15 years, but this time, we actually could get there!


love this news!!! Thanks so much, and thanks for your participation in all things diabetes related. You are my go to for the latest and greatest information!
Thanks Ken! We’re grateful to help in any way we can!
Seems like if the patients own stem cells were used, rejection wouldn’t be a problem. Of course that would be very customized, time consuming in production, and expensive.
Yes, and unfortunately there’s not enough of these islet cells in one person to affect diabetes. Before we could synthesize them, it took 20-30 cadavers to get enough islet cells to make one person insulin independent.
Problem is in T1s, the adaptive portion of the immune system generated antibodies to beta cells. So even if beta cells were generated from one’s own cells (like the chemically induced stem cells in Chinese trials) it’s likely these antibodies would still recognize antigens on these stem beta cells and work with immune t cells to attack them. However, the innate portion of the immune cells (macrophages) wouldn’t eat these beta cells because they aren’t foreign. So in theory, not as many gene edits would be necessary if the cells are coming from the same patient and at least some of the immune cells could perform surveillance of any stem beta cells that developed deleterious mutations and could attack/eat them – right fully so for once in T1s.
Dr. Edelman,
Question, why wouldn’t chemotherapy work initially when beta cells are in the stage of being depleted by virus etc. My son had central nervous system vasculitis from a potential virus and was given chemo or die.(one can actually read his story in “the books”. It worked great. Just wondering if a chemo drug could stop the proliferation and reset the autoimmune system to stop attacking the beta cells.
Hi Glynis,
It’s a great thought, but unfortunately no, it would not help. People have tested it.
If these transplanted islet cells are somehow “masked” from the immune cells (T cells) that attack them in an autoimmune response – is it possible that the implanted islets could give rise to cancer? Could mutated islet cells proliferate if not recognized and destroyed by the TID’s immune system? Sean, above, remarks that these stem beta cells would still have some immune response to mutant cells. What is the research on this?
Judy, I’ve read the cancer risk is there but low. These types of cells are not typically associated with cancers and the screening process for cells going in is intense. Animal studies haven’t shown much oncological risk either. Patients would likely need to get an MRI periodically to look for signs of cancer and I believe the cells could be killed off if necessary by introducing an antibody that can recognize and neutralize them.
Yes, this is a concern. The immune system is very important in eliminating cancerous cells, so another reason why this approach is taking time and considerable amounts of research to get right.
Thank you so much for creating such an informative and easy to understand report!
I can’t wait for the cure!
Us too! 🙂
Will this work for a type one diabetic without a pancreas? I had mine removed this past December along with my spleen due to a pre-cancerous tumor
Yes it would.
If these larger drug companies are getting involved , it means that see a revenue stream .
That being said a cure might be coming but only the 1% will be able to afford it
That makes it more depressing to know that a cure will become available but only the rich will be getting it.
Unless a firm patents it for a $1 and provides it to the world will at that cost will the masses be able to participate !!
Wait isn’t that what the discovers of insulin did !!
Some people ( without insurance ) are paying $400-$500 a vial .
The pessimist in me is just being a realist
We can’t predict the future, and its generally the case that new therapies (in any field of any type) are typically expensive. However, if we truly had a cure, that would save insurance companies billions in avoiding paying for insulin, pumps, complications such as surgeries, dialysis etc. So we are optimistic that these curative approaches would be covered by insurance.
Exactamundo!
This is so exciting I am so thankful for the research . Iv been t1 for 35 years. My brain can not process the thought of not having this disease
After living with it for so long it’s hard to wrap your head around, but we are up for the challenge!! 🙂
I hope to see it in my lifetime. I have had it 65 yrs and am starting to show some resistance. Let’s hope Medicare covers it?
Yes we hope so too!🤞
I hope a cure finally happens and one that does not require immunosuppressants! I have been a T 1 D for 46 years!!!! It’s about time!!!
Would it be possible to use stored stem cells from the cord and blood following the birth of your baby if stored privately?
Hi Julie,
We don’t need to do that anymore because we can synthesize them, and they’re more pure and easier to manipulate.
This is amazing news praying for a cure! My daughters 14 and was diagnosed with type 1 last year. So thankful For your work!!
Thanks Tracey! We are excited too! FYI, we will be launching some educational resources specifically for teens in the coming months. Stay tuned! 🙂
What would best possible islet cell therapy for me ?I am 79 yo and have T1 for 50 yrs .I received a kidney transplant 10 yrs ago and it is doing well on immunocompromised meds .My daughter stored my granddaughters cord blood in hopes it could be used .So what would be best therapy for me .
Thanks
Hi James,
The islet cells that Vertex uses are derived from stem cells in a lab, so the therapy for you would be no different than everyone else. Those cord samples aren’t really going to help in these situations.
I’m 68. 47 of them I’m type1. When I read this I cried. I thought maybe I would be able even several years to live without injection. Thank you everyone who worked on this project. God bless you.
It’s pretty incredible to think about. 🙂
I am a type one diabetic now at age 81, I’ve been a type two for at least 20 years, controlled with diet and exercise. But in 2021 I had Covid and received the injection for it and did well but evidently the auto immune response kicked me into a type one diabetic. Still figuring out how much insulin to take every day. I go to a diabetic endocrinologist and have my third visit next month. It would be fantastic if the stem cell theory worked along with without having to be on an auto immune. . Still figuring out how much insulin to take every day. I go to a diabetic endocrinologist and have my third visit next month. It would be fantastic if the stem cell theory worked along with without having to be on a auto immune suppression drug.. thank you for all you do.
Hi Catherine,
Hope your endo can help you with insulin amounts. It’s a lot of trial and error, but this may help also:
https://tcoyd.org/2021/05/how-do-i-know-how-much-insulin-to-take-with-each-meal/
Take good care!
I live in RI and have lived with T1 fit 67
You are what we call a diabetes legend, Donna!
Thank you for this “dubious “ honor! T1 for 67 years! Surprisingly, I’ve lived a full life with the help of my 5 children. My “healthy husband, died in 2022 of a stroke! Life certainly isn’t always easy, equal or fair but we must make the BEST with what we’re given! My A1C has stayed a consistent 5 to 5.2! I worked a 38 year HS teaching career with 4 years of perfect attendance despite the fact that my kids were often sick! I hope and pray that I can be cured of T1!
We hope so too, Donna! Thank you for being part of the TCOYD family for so long! 🙂
What will be the source of the stem cells?
Hi Sharon,
They are synthesized in a lab.
Thank you. You are brilliant scientists. I am Type 1 diabetic LADA. Got it age 52. Am now 70. Praying for a cure. I will participate in clinical trials. One rejected me in Boston 8 years ago. Took a train from NJ to Boston. Got bloodwork. Was told I was they wanted someone newly diagnosed. I told them I had it by phone Great disappointment. Thank you. Let’s pray for a cure. Especially for the children. God bless all of you researchers, doctors, scientists who are working on a cure for this insidious disease.
Thanks Donna. We hope it happens soon too.
Type 1 diabetes is a trillion dollar industry.
Big Pharma will not allow this cash cow to be slaughtered.
As the CEO of Pfizer stated ” There is no profit in curing anything”.
I have RA and have been on a biologic for many years. I also am a breast cancer survivor (chemo and radiation). I would like to be part of a study but these factors exclude me. Will I be eligible for a stem cell transplant when it becomes available?
*T1D for 45 years and I am hopeful for a cure!
You should be! In most studies they have to stick to strict inclusion criteria, but you should be eligible.
“Only 5 more years……” I been hearing this for the past 45 years.
Us too!! 🙂