
- Type 2 diabetes can change and progress over time – it’s simply the biology of type 2 diabetes unfolding.
- Newer medications like GLP-1s and SGLT2s have been game-changers for type 2 diabetes management. GLP‑1 medicines help to curb appetite, lower A1c, and protect the heart. SGLT‑2 medications make you “pee out” extra glucose while shielding kidneys and reducing heart‑failure risk.
- Adding new medications to your diabetes regimen isn’t a sign that you failed at diabetes management. Utilizing multiple therapies can help to delay or prevent complications.
- Lifestyle is still important. Exercise, nutrition, stress reduction, and quality sleep can amplify medication power and keep your A1c’s cruise control set lower for longer.
Reading Time: 5 minutes
Wait…type 2 diabetes is progressive? Yep, type 2 diabetes isn’t a one-and-done diagnosis—it actually evolves over time. Many people start with lifestyle tweaks and a single pill, feel like rock stars for a few years, and then—bam!—the A1c creeps up and a new med (or even insulin) is sitting in your medicine cabinet.
But that isn’t actually a bad thing, and we all need to do a better job of reframing the T2 narrative: needing more medication isn’t proof you “messed up.” It’s simply the biology of T2D unfolding.
Why Type 2 Diabetes Progresses
In the simplest terms, type 2 diabetes is always progressing. Long before anyone sees an elevated A1c, two problems are brewing:
- Insulin resistance—your muscles, liver, and fat cells stop responding to insulin.
- Beta-cell fatigue—your pancreas tries to respond to the resistance by pumping out extra insulin, but over the years those cells tire out and production drops.
Genetics drives a lot of this. A significant percentage of people with type 2 can point to at least one close relative who walked the same path. Researchers have identified dozens of “suspect genes,” each nudging insulin resistance a little higher.
That brings us to the so-called “thrifty-gene” effect—ancestral DNA that told our bodies to hoard energy during feast–famine cycles. This “thrifty-gene” sets up many people with a recipe for high blood sugar in a modern world full of desk jobs and drive-thru windows.
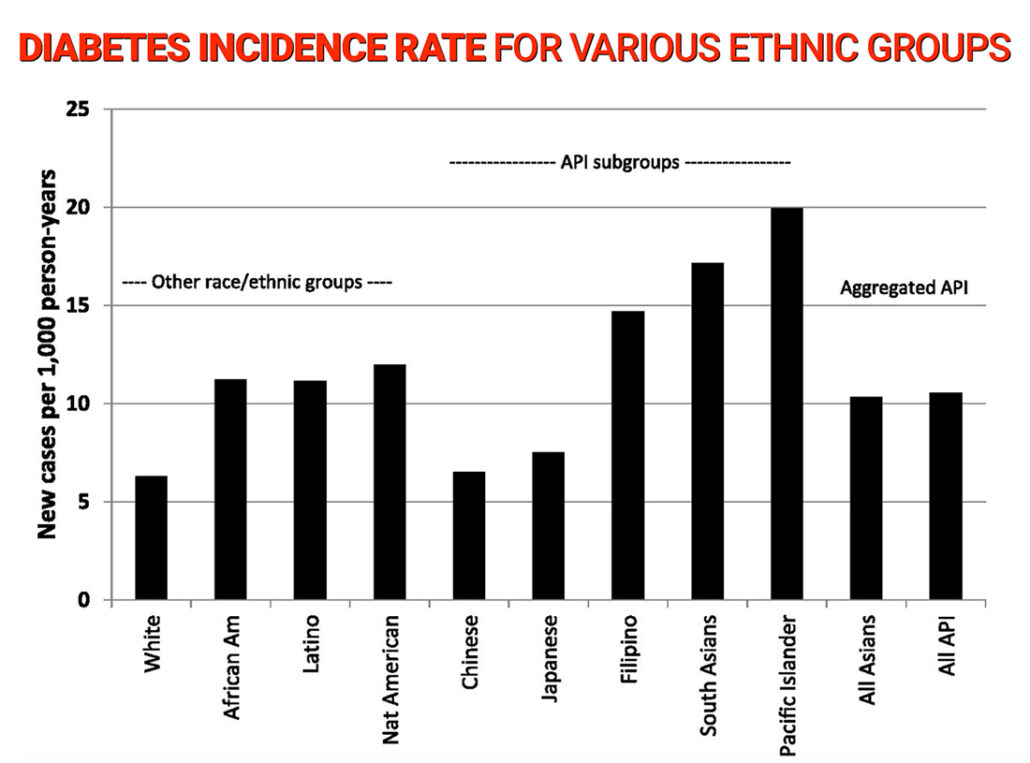
Certain ethnic groups, including Hispanic/Latino, Black, Native, Pacific Islander, and many Asian populations inherit a heavier dose of this genetic baggage, which partly explains the higher rates of type 2 in those communities.
Unfortunately, even when someone eats reasonably well and exercises, their pancreas may still be working overtime. Gradually, glucose sneaks upward, and the care plan has to evolve.
Let’s Two-Step With T2D
Get out those dusty disco pants from the closet. Think of early type 2 as a nightclub. At first, the DJ (your pancreas) cranks the volume and insulin levels skyrocket. Blood sugars might look only mildly high on lab work, but out there on the dance floor, insulin is five to ten times normal. That keeps the dance party going for a while.
Eventually, the DJ blows out his speakers. Years of over-production leave fewer healthy beta-cells, so insulin output drifts downward just as resistance stays high. Now glucose really piles up in the bloodstream. It’s why someone can coast with “borderline” numbers for years and then, seemingly overnight, land in the 200 mg/dL club.
This isn’t anyone’s fault—it’s the natural arc of the disease. The goal of type 2 diabetes management is to slow that arc by easing insulin resistance, protecting beta-cells, and adding medications when the pancreas starts nodding off in the DJ booth.
T2 Treatments: From ’90s Playbook to Modern Game-Changers

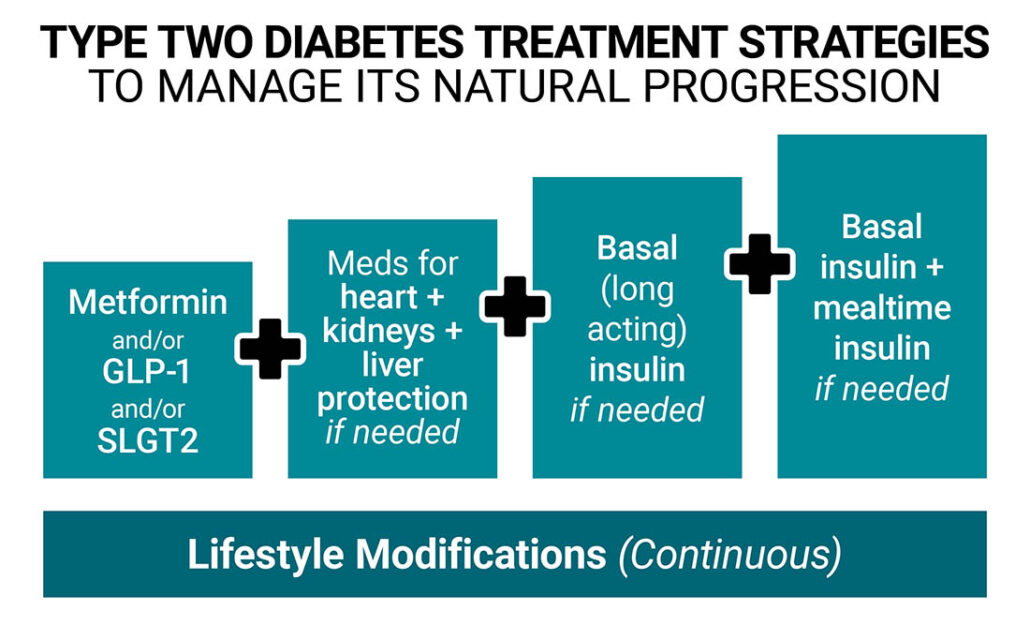
Back in the early 1990s, treatment was basically to start metformin, add a sulfonylurea, and graduate to insulin. That plan worked, but it didn’t directly tackle weight gain, heart risk, or kidney decline.
However, in the early 2000s, two incredible type 2 diabetes medications entered:
GLP-1 Receptor Agonists (Ozempic® & Mounjaro®, etc.)

This hormone tells beta-cells to release insulin only after eating (and only if the glucose value is high), slam the brakes on glucagon, slow stomach emptying, and dial down appetite. That means better post-meal numbers and meaningful weight loss. They also lower the fasting glucose level (the value first thing in the morning). Cardiologists now prescribe them routinely before (for prevention) and after heart attacks because they lower cardiovascular events. Even kidney doctors are starting to use them to reduce the progression of kidney disease.
SGLT-2 Inhibitors (Jardiance®, Farxiga®, etc.)

These medications send excess glucose out through your kidneys – you literally pee out sugar. They can also lower blood pressure, produce modest weight drops, and provide protection for the heart (especially congestive heart failure) and kidneys. Approved in 2014, SGLT-2 inhibitors are now being prescribed by doctors across several specialties.
Thanks to these and newer combo therapies, many people now hold an A1c under 7% with fewer lows, less weight gain, and even delayed need for insulin.
Why “More Meds” Isn’t a Bad Thing
If your doctor adds a second (or fifth) medication, it doesn’t mean you flunked on your diabetes management. Using multiple drugs early can delay—or sometimes avoid—full-scale insulin therapy, preserve remaining beta-cells, and lower the risk of heart or kidney complications. It’s better to be the person with a 6.8 % A1c on five meds than the person at 9% proudly bragging about taking none.
Think of it this way: If your car needs new brake pads, you don’t blame the driver—you fix the brakes.
Lifestyle Makes a Difference
Modern drugs are amazing, but they still need dedication on your part. Here’s the short version of every “lifestyle” lecture you’ve ever half-heard:
Move Your Muscles

10 minutes of brisk walking after meals helps move extra glucose out of the bloodstream. Choose whatever you’ll actually do: pickleball, yard work, Beyoncé dance-along videos — your pancreas can’t tell the difference, it just enjoys the help.
Mind Your Menu

You don’t have to marry kale, but try swapping some refined carbs for veggies, proteins, or healthy fats. Think breakfast tacos on high-fiber tortillas instead of sugary cereal. Or go with roasted chickpeas instead of chips. Small edits beat unrealistic overhauls.
Sleep and Stress Matter

Skimping on sleep or living in permanent Zoom-meeting panic pushes cortisol up, which pushes glucose up, which pushes you up the medication ladder faster. A 20-minute walk, a breathing app, or lights-out 30 minutes earlier can shave points off fasting sugars.
None of this is about perfection. It’s about taking the little steps that matter.
Frequently Asked Questions (FAQ)
💊 What is the first-line treatment for newly diagnosed type 2 diabetes?
Most guidelines still start with lifestyle changes plus metformin, because metformin lowers A1c 1-2 points, is inexpensive, and rarely causes weight gain. If a person already has heart, kidney, or weight concerns, many doctors now add a GLP-1 or SGLT-2 right from the start.
💉 How long does it take for type 2 diabetes to require insulin?
There’s no fixed timeline. Some people need basal insulin at diagnosis, while others stay off insulin for decades. Early use of combination medications or injections – along with weight-loss-focused lifestyle changes – can delay or even avoid the need for insulin. But remember, going on insulin doesn’t mean you failed in your type 2 diabetes management.
💖 Do GLP-1 medicines really protect the heart?
Yes. Large outcome trials show GLP-1 receptor agonists reduce major cardiovascular events (heart attack, stroke, CV death) by 12-26% in people with type 2 diabetes and established heart disease.
🩺 Can SGLT-2 inhibitors help diabetic kidney disease?
Absolutely. Drugs like Jardiance® and Farxiga® lower the risk of dialysis, slow eGFR decline, and cut hospitalization for heart failure. These benefits are even seen in people with moderately reduced kidney function.
Key Takeaways
- Type 2 diabetes is progressive, but many people with T2D live just as long or longer than those without. If you take your diabetes management regimen seriously, you can live just as well or better than anyone else.
- Using multiple therapies isn’t a sign of failure, and it can be a powerful treatment approach.
- Lifestyle modification is huge. Consistent movement, smarter carbs, quality sleep, and stress management are steps you can control.
Need more guidance? Check out our Video Vault or browse our articles in the archive. Knowing the science (with a laugh or two) keeps you informed and in control of treating your diabetes.

I got week on Ozempic and could not use Mounjaro cause it locked me up way too much. I used to take Victoza but that is discontinuing. Can I use Trulicity? Since i stopped Mounjaro and Ozempic and Victoza my blood sugar range has not been higher than 60. I would like to take s GLP. Is there one other available I can try? Also I have Kidney disease and Farxiga and Kenedria are great can I add another SGLT-2 to this like Jardiance? I want to have my Kidney disease imporve and I walso would like to get my blood sugar range back about 80 like when I used Qzempic.
thanks you for any info you can give me and I definitely woudl consult with my Dndo before changing anything
Erv Nerius
It’s extremely unusual for people not to be able to tolerate Ozempic and Mounjaro, and I would be afraid that you would have another adverse event with another GLP-1. However, you can always try Trulicity because they are all a little bit different, and just start with the lowest dose. Regarding your kidney question, do not add another SGLT-2 if you are already on one. One is enough, and two will be too much.