
- Men over 50 with diabetes face a higher risk of developing prostate problems. Factors like insulin resistance, chronic inflammation, nerve damage, and vascular disease all play a role, and chronically elevated blood sugar levels over many years can make each condition worse over time.
- Poorly controlled diabetes can affect circulation. Reduced blood flow to the prostate can irritate and damage the gland, which can stimulate growth. This can lead to a condition called benign prostatic hyperplasia (BPH).
- Symptoms of an enlarged prostate include making multiple trips to the bathroom, difficulty starting to urinate, discomfort or pain when urinating, a weak urine stream, and feeling like your bladder never fully empties…because it doesn’t!
- Diabetes and urinary problems are common, but treatments exist. Treatments for an enlarged prostate include medications to shrink or relax the prostate, minimally invasive procedures, and surgery.
Reading Time: 5 minutes
After my most recent prostate exam, the doctor left the exam room and the nurse came in. As she shut the door, she turned to me and whispered, “Who was that guy??”
If you are a man over 50, prostate exams will be in your future…hopefully with a real urologist.
And if you are a man over 50 with diabetes, guess what…you’re at a higher risk for prostate problems. (Just add that to the ongoing list of stuff we have to deal with!) Why are diabetic men more at risk? Well, urine luck 😉…we’re about to shed some light on the subject.
What Is the Prostate, Anyway?
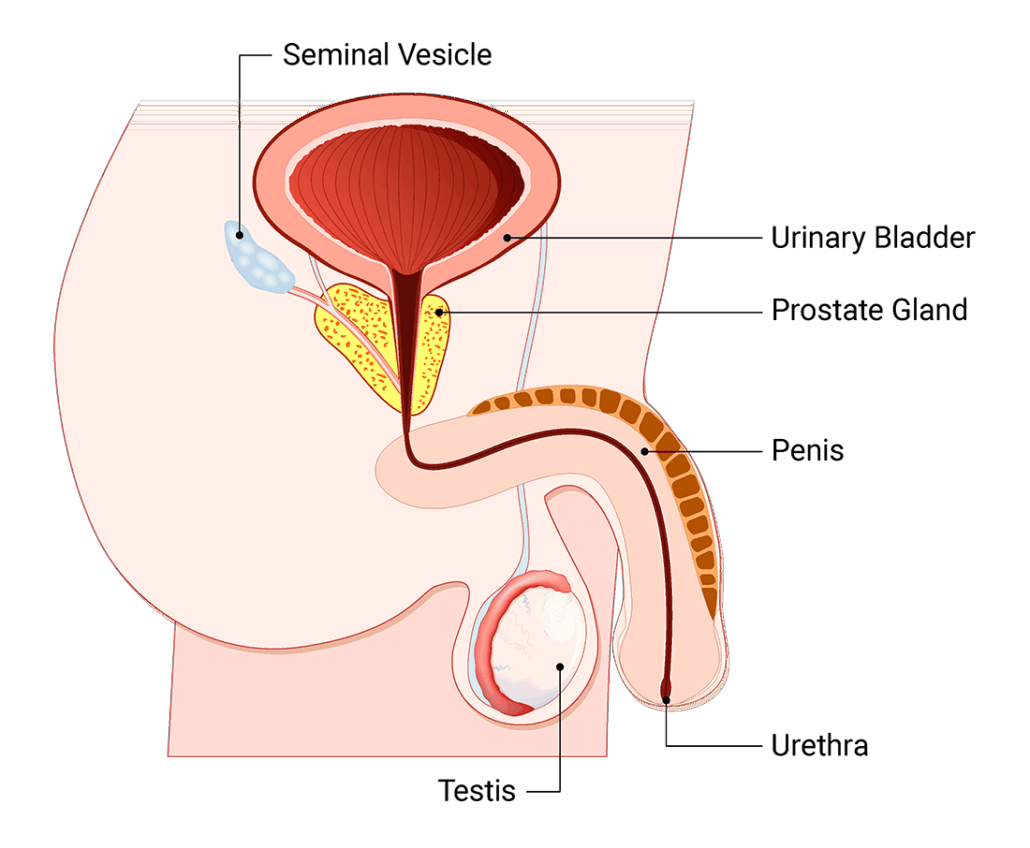
We’ve all heard of it, but does anyone really know what it is or what it does? The prostate is a small gland in the male reproductive system that’s about the size of a walnut. It sits just below the bladder and surrounds the urethra, which is the tube that carries urine and semen out of the body (and all over the sheets!). The prostate’s main job is to make the fluid that helps keep sperm happy and healthy during, well, you know – baby-making time. The prostate also helps control urine flow.
Diabetes and Urinary Problems: Why Are Men with Diabetes at Higher Risk for Prostate Issues?
As all men get older – usually after the age of 50 – the risk of prostate problems goes up. It’s just a fact of life, and could be related to lower testosterone levels.
But men with both type 1 and type 2 diabetes have an even higher risk. This may be due to factors like insulin resistance, chronic inflammation, nerve damage, and vascular disease, all made worse by chronically elevated blood sugar levels over many years.
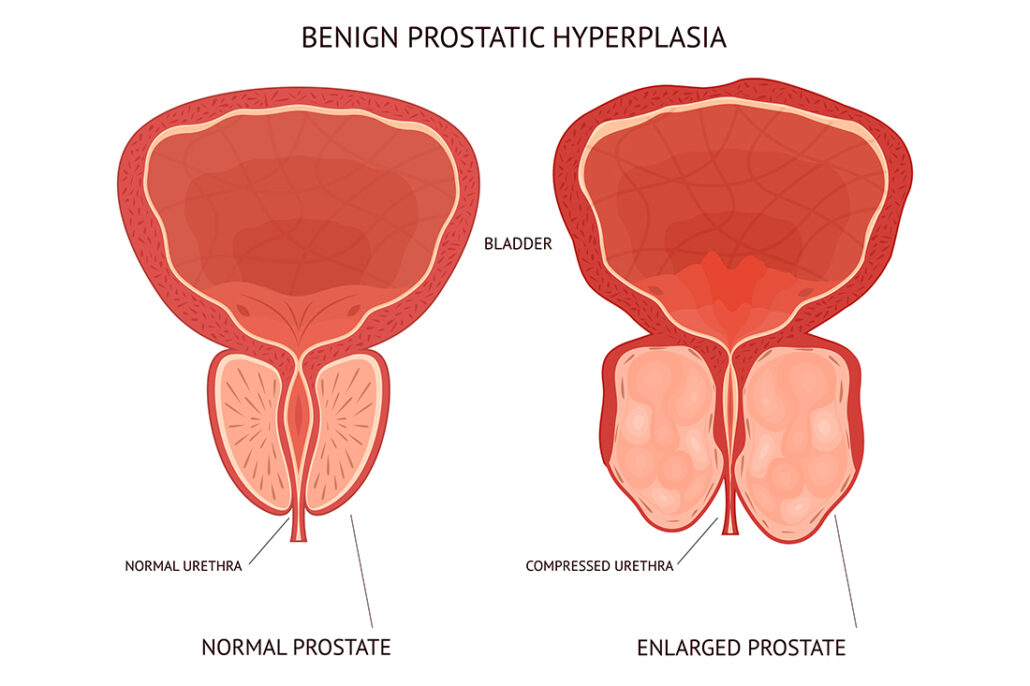
Because poorly controlled diabetes can affect circulation, reduced blood flow to the prostate can irritate and damage the gland, which can stimulate growth. This can lead to a condition called benign prostatic hyperplasia (BPH), which just means an enlarged prostate that’s not cancerous. However, an enlarged prostate can lead to problems in the bladder, urinary tract, and kidneys.
Diabetes can sometimes make it harder to catch and monitor prostate problems because men with diabetes often have lower PSA levels, which can mask early signs of BPH and cancer.
PSA levels refer to the amount of prostate-specific antigen is in the blood, which is a protein produced by both normal and cancerous prostate cells. The PSA test is used to screen for prostate cancer and to help diagnose or monitor other prostate conditions.
Digging Deep: What Are the Symptoms of an Enlarged Prostate?

When the prostate is enlarged, it squeezes the urethra (the tube that carries urine from the kidneys to the bladder), and that pressure can bring on some pretty uncomfortable (and annoying!) symptoms.
Common symptoms include:
- Difficulty starting to urinate
- Leaking or dribbling urine
- A weak or slow urine stream
- Making multiple trips to the bathroom in the middle of the night
- Feeling like your bladder never fully empties…because it never empties!
So basically, it can affect almost everything before, during, and after you go to the bathroom.
And if your diabetes is not in good control and/or you have metabolic conditions like central obesity, high blood pressure, and high triglycerides, that can make symptoms worse.
Having a neurogenic bladder can also impact symptoms of BPH. A neurogenic bladder is a form of autonomic neuropathy where the muscles of the bladder don’t compress normally, so it’s harder to empty the bladder fully.
Getting to the Bottom of Things: How BPH Is Diagnosed (try to find a doctor with small fingers!)

If you’re spending more time in the bathroom than usual – and staring at the toilet with nothing happening – your prostate might be trying to tell you something.
Getting checked for BPH is pretty straightforward. Your urologist will ask you some questions, run a few tests, and probably have you drop your pants for that awkward exam that’s the “butt” of so many jokes. The good news is it’s over pretty quickly – even the doctor doesn’t want to hang around in there for too long.
Here’s what to expect at the urologist’s office:
Medical History and Symptom Check: Your doctor will ask about your symptoms, how long you’ve had them, and how much they affect your daily life. You may also fill out a questionnaire called the International Prostate Symptom Score (IPSS), which helps measure severity.
Physical Exam: This often includes the digital rectal exam. By feeling the prostate through the rectal wall, your doctor can estimate its size and check for anything unusual, like masses.
Urine and Blood Tests: Urine tests can rule out infections or other causes of your symptoms. Blood work may include a PSA test since BPH and cancer can sometimes look similar symptom-wise.
Additional Testing:
Additional tests may include:
- Uroflowmetry to see how strong your urine stream is and how much urine you pass
- Post-void residual test (conducted with an ultrasound) to check how much urine stays in your bladder after urinating
Double Trouble? The Diabetes and Prostate Cancer Connection
The connection between diabetes and prostate cancer is complex – some studies suggest that men with long-term type 2 diabetes may actually have a slightly lower risk of getting prostate cancer, possibly due to lower circulating testosterone and altered PSA levels.
However, if prostate cancer does show up in someone with diabetes, it can be more aggressive and harder to treat (particularly in men with poor diabetes control) because metabolic disturbances and chronic inflammation may support cancer progression.
This is one reason why screening is so important, along with good diabetes control.
How to Go with the Flow When It Comes to Diabetes and Urinary Problems: Prevention, Management, and Treatment
So your walnut-sized prostate is now the size of a lemon? Don’t sweat it…you’re not alone, and there are lots of treatment options available. Therapies range from lifestyle tweaks to surgery, and there’s even one special medication with unexpected benefits that can turn your prostate lemon into lemonade.
- Get Regular Check-ups: Get regular check-ups and screenings with your primary care doctor (and a urologist if needed) to monitor prostate health and catch problems early.
- Watch for Symptoms: Pay attention to urinary frequency, urgency, stream trouble, and the amount of nighttime trips to the bathroom, and talk to your provider if they worsen.
- Glycemic Control: Keeping your blood sugars in a healthy range can help lower the risk of inflammation and circulatory problems that contribute to prostate enlargement.
- Lifestyle Choices: Sometimes, small adjustments make a big difference. Cutting back on evening fluids, limiting caffeine and alcohol, and exercising regularly can reduce urinary symptoms. Losing weight and quitting smoking can also improve overall prostate and bladder health.
- Medications: Doctors often start with medication to shrink the prostate or relax the muscles around it. Common choices include: Alpha blockers (like tamsulosin, also called Flomax) to relax the muscles and improve urine flow, 5-alpha reductase inhibitors (like finasteride) to shrink the prostate over time, and sometimes, a combination of the two.
- Minimally Invasive Procedures: If medicines don’t cut it, office-based treatments can help. Options like UroLift (tiny implants that hold the prostate open) or Rezum (steam therapy that shrinks prostate tissue) can improve symptoms without major surgery.
- Surgery: For severe symptoms or when other treatments fail, surgery may be recommended. The most common is TURP (transurethral resection of the prostate), where extra prostate tissue is removed. Newer surgical techniques may also be available depending on your health and the size of your prostate.
One Pill, Two Thrills
Believe it or not, sometimes doctors will prescribe a low dose (5 mg) of daily Cialis (tadalafil) to help relax the muscles in the prostate and bladder. This helps urine flow more freely, and it keeps other parts of you ready to rise to the occasion if the mood hits. Since men with diabetes are three times more likely to develop erectile dysfunction than those who don’t have diabetes, this could help kill two birds with one stone. Daily Cialis really works – and no need for a towel rack!
Frequently Asked Questions
💦 Is there a link between diabetes and urinary problems?
Yes, diabetes can increase the risk of urinary problems like overactive bladder (sudden urges to pee and leaking), trouble fully emptying the bladder, urinary tract infections (UTIs), and having to make multiple trips to the bathroom, especially at night. This may be due to increased insulin resistance, inflammation, nerve damage, and vascular conditions caused by chronic high blood sugars or poor glucose control over the long-term.
🩸 What’s the connection between blood sugar and inflammation?
Chronically high blood sugar can cause inflammation in the body. When blood sugar stays elevated for long periods of time, it can trigger the body’s immune system to produce inflammatory chemicals. This ongoing low-level inflammation can damage tissues and worsen insulin resistance.
🧐 Why are men with diabetes more at risk for urinary tract infections (UTIs)?
There are a few reasons. First, high blood sugars can cause more sugar to be present in the urine, and bacteria love this sugary environment to grow. Second, diabetes can damage the nerves of the bladder wall, making it harder to fully empty. When urine stays in the bladder too long, bacteria have a chance to grow and cause infections. Third, poorly controlled diabetes can weaken the immune system, which means the body is not as good at fighting off infections, including UTIs.
Key Takeaways: Diabetes and Prostate Health
Benjamin Franklin should have said that the only certainties in life – for men at least – are death, taxes, and a bigger prostate.
If you have an enlarged prostate, the good news is you’ve lived long enough to get one. Half of all men over 60 will develop this condition, and by the age of 85 that number goes up to 90%.
Even though BPH is super common – especially in men with diabetes – you don’t have to just “live with it”. Your doctor can tailor a treatment plan for you to help improve your symptoms.
Getting regular screenings, addressing symptoms early, and following a comprehensive care plan can ease discomfort, protect your quality of life, and help prevent complications.
No one looks forward to a prostate exam, but hey, at least that fingerprick only happens once a year!
Explore our resource library and video vault, and subscribe to our monthly digital newsletter for more tips, tools, and expert guidance on how to take control of your diabetes.

This an outstanding article. It describes very clearly the problems and challenges that I have experienced these past 15 years. I have type I diabetes ( 45 years) and underwent radaition treatment for prostate cancer (10 years ago).
Thanks for sharing Max, and hope you’re doing well.