
- Diabetic ketoacidosis (DKA) is a serious and potentially life-threatening complication of diabetes, but it is preventable and treatable.
- Elevated ketones can lead to DKA. When the body doesn’t have enough insulin and starts using fat as fuel, this leads to the production of ketones. Too many ketones can cause the blood to become dangerously acidic.
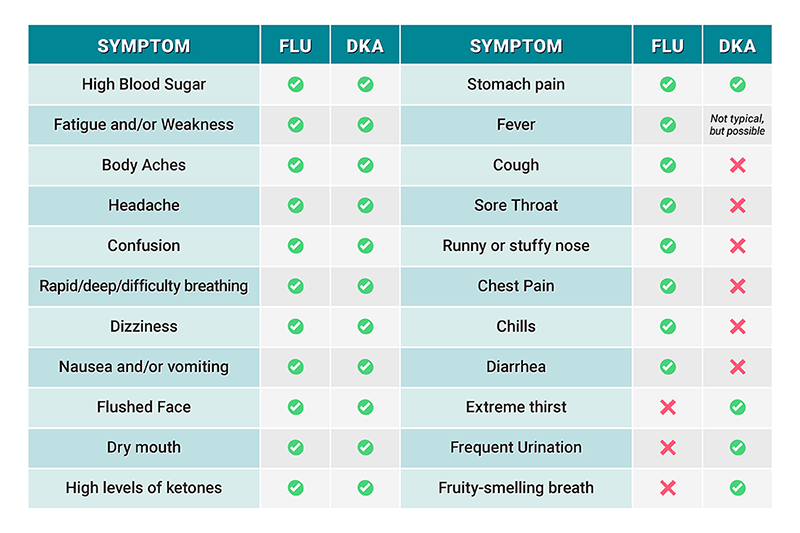
- Symptoms of rising ketones and DKA can be very similar to the flu. This makes it easy to confuse the two, potentially delaying important early treatment if it is DKA.
- Testing your ketones with a blood ketone meter is the best way to know if your ketones are rising and you are at risk of DKA. Urine ketone tests are also available, but they do not measure beta-hydroxybutyrate, which is the predominant ketone present in DKA.
- Treating DKA requires insulin, hydration, and sometimes carbs (depending on glucose level), but if you’re vomiting and you can’t hold anything down, you need to go to the ER.
- DKA prevention starts with education and planning. Learn the ambiguous warning signs, create a DKA plan with your healthcare team, and keep extra insulin, unexpired ketone test strips, fast-acting carbs, and sugar-free fluids on hand.
Reading Time: 7 minutes
Fall is in full swing, which means the air is crisp, flannel is in fashion, and pumpkins are finding their way into foods where they don’t belong.
It’s also the start of flu season, and when that first symptom hits, you know what’s coming… headaches, body aches, GI issues, and feeling like you’ve been tackled by a linebacker.
But if you live with diabetes, those familiar symptoms could actually signal something much more serious – diabetic ketoacidosis, or DKA. So how do you know if your symptoms are DKA or flu…or both? Let’s break it down.
What Is DKA?

DKA is a serious complication of diabetes that occurs when your body doesn’t have enough insulin to move sugar into your cells for energy. This can happen if you lose access to insulin for any reason, like if your insulin pump infusion set (or site) is not working and insulin delivery is not happening.
Without insulin, your body starts breaking down fat for fuel, which leads to ketone production. A small amount of ketones is generally not a problem, but if the ketone levels get too high, they make your blood way too acidic. Rising ketones are your body’s way of waving the red flag when insulin is too low and you’re on your way to DKA. Left untreated, DKA can be life-threatening.
Many people are first diagnosed with type 1 diabetes while in DKA, and hopefully they never experience it again. But about 5–8% of adults with T1D still end up in DKA every year. And while it’s much more common in type 1 diabetes, people with type 2 diabetes don’t get a free pass. DKA can happen there too if you’re on insulin and/or taking certain medications like SGLT2 inhibitors.
What Causes DKA?
The top culprits are illness and insulin delivery issues, but here’s a detailed breakdown of the primary DKA causes:
- Not enough insulin, or no insulin at all: Missing insulin doses, taking less insulin than your body needs, using expired insulin, insulin pump failure, or any type of infusion set or infusion site problem
- Illness or infection: Illnesses like the flu, pneumonia, urinary tract infections, stomach bugs, etc. can raise your body’s stress hormones, making insulin less effective (when you’re under stress, you need more insulin)
- Certain medications: SGLT2 inhibitors (Jardiance, Faxiga, Invokana, Brenzavvy, Inpefa) and certain steroids
- Other medical events: Heart attack, stroke, pancreatitis, surgery
DKA Symptoms (and How They Can Feel Like the Flu)
In a recent study, 46% of people with type 1 diabetes couldn’t name a single DKA symptom. Without cheating and looking at the list below, can you?? It’s important to know the warning signs because DKA can escalate quickly.
Early DKA Symptoms Include:
- High blood sugar levels (usually above 200 mg/dL)
- Muscle aches, muscle stiffness, body aches, cramps
- Fatigue or weakness
- Extreme thirst or very dry mouth
- Frequent urination
- Brain fog
- High levels of ketones
Severe DKA Symptoms Include:
- Rapid breathing, deep breathing, or difficulty breathing
- Flushed face
- Fruity-smelling breath
- Headache
- Confusion
- GI symptoms like stomach pain, nausea, vomiting
As you can see, DKA can look a lot like the flu. Knowing the key differences can help you catch DKA early before it becomes an emergency situation.
Comparison of DKA and Flu Symptoms
So How Do You Know If You Have the Flu, DKA, or Both?
One of the more telling signs that you are in DKA and not the flu is fruity smelling breath, but if you’re experiencing other symptoms (and no one is there to tell you your breath smells like a kumquat) what do you do?
You need to test your ketones.
Everyone with type 1 diabetes – and people with type 2 diabetes on insulin or SGLT2 medications – should have a ketone meter and unexpired test strips. You can find ketone meters and test strips at the pharmacy or on Amazon (keep in mind, sometimes you have to buy the meter and strips separately).
Blood ketone meters are preferred because urine ketone tests aren’t as accurate. Urine ketone tests only detect acetoacetate and do not measure beta-hydroxybutyrate, which is the predominant ketone present in DKA. This is what limits their accuracy.
If you’ve never used a ketone meter, check your ketones a couple of times when you’re feeling fine just to get an idea of what your typical baseline value is, and to get familiar with how to use a ketone meter.
DKA and Ketones: When Should You Test?
Most people don’t check for ketones nearly as often as they should. In fact, about 64% of people with type 1 diabetes either rarely test, or have never tested at all. Healthcare professionals may not always prescribe ketone tests or suggest them. Skipping these checks can be risky.
Here’s when to pull out the meter and test strips:
- When you’re sick, especially if you’re vomiting, have stomach pain, or a fever (and yes, test even if your blood sugar isn’t high)
- When you have prolonged blood glucose elevation (over 200 mg/dL for several hours) and are resistant to the glucose-lowering effects of insulin
- When insulin delivery is in question: clogged pump tubing, a dislodged infusion site, or a dislodged patch pump
How to interpret blood ketone level results:
- Normal: less than 0.6 mmol/L
- Elevated: levels between 0.6 and 1.5 mmol/L (test again in 2 hours)
- High: levels between 1.6 and 2.9 mmol/L
- Urgent High: levels above 3.0 mmol/L
If your level is over 1 mmol/L, that’s when you’re getting into a problem area. If you can self-treat, follow the procedures below, but if you are vomiting, have difficulty breathing, or cannot self-treat for any reason, follow your HCP’s guidance, call 911, or go to the ER.
How Do You Treat DKA?
If you’re able to hold down food and liquids, here’s how to treat DKA in order to avoid a visit to the ER and/or hospitalization:
- Stop taking an SGLT2 inhibitor if you’re on one.
- Give yourself insulin. The recommendation is to give yourself a correction dose of insulin that’s 1.5 times your usual dose (or increase insulin dose per your healthcare provider’s guidance). Everyone’s needs will be different. Insulin should be taken at the same time as the carbs and fluids mentioned below. It’s important to know that when you’re in DKA, your body is resistant to insulin. If you wear an insulin pump and there’s a chance you have an infusion set or infusion site problem, use fast-acting insulin from a pen or syringe. Then change the infusion site location for your pump so you’re still getting basal insulin.
- Consume carbs. If glucose is less than 250 mg/dL (or otherwise directed by your HCP), eat or drink about 30 grams of fast-acting carbs (juice, gummy bears, regular soda, regular Gatorade, glucose tabs, etc). It might feel counterintuitive, but carbs help shift your brain’s fuel source from ketones back to glucose, which stops your body from making more ketones.
- Hydrate. Drink no/low calories liquids like water or sugar-free, caffeine free sports drinks with electrolytes to help flush the ketones out.
Important to note: a 12 oz can of Gatorade does have 50 mg of potassium, so if you’re on a potassium-restricted diet you should check with your healthcare provider before taking it.
When it comes to treating DKA, the faster you intervene, the faster you will get better, though it may take several hours. And you cannot forget to take carbs and insulin because that turns off the brain’s drive to produce ketones.
Continue to check your glucose and your ketone levels at least every hour. Keep bolusing every one to two hours until your glucose starts to come down and you feel better.
Understanding Euglycemia DKA: You Can Be in DKA Even If Your Glucose Is Normal
There is a fairly common variant of DKA called euglycemic DKA when glucose levels aren’t super high. They could even be below 200 mg/dL! In the recent past, the commonly accepted criteria for DKA was above 250 mg/dL, but because of euglycemic DKA they lowered it to 200 mg/dL. Certain medications like SGLT2 inhibitors can cause euglycemic DKA to occur. Euglycemia DKA follows the same treatment protocol mentioned above.
When to Seek Medical Treatment
When it comes to treating DKA, if you’re vomiting and you can’t hold anything down, you’re not going to be able to self-treat or get better on your own. You need to go to the ER because they can give you fluids and insulin through an IV line.
How to Prevent DKA
Preparation and education are the best ways to keep DKA at bay. If you have type 1 diabetes – or type 2 diabetes and you take insulin or an SGLT2 inhibitor – here’s how to prevent DKA and lower your risk:
- Know the warning signs. Learn the symptoms of rising ketones or early DKA so you can address them before things get serious.
- Check your ketones when needed and know what the numbers mean. A quick ketone test can help you decide your next move.
- Create a ketone management game plan with your healthcare team. General guidelines are listed below.
- Keep a backup stash of diabetes supplies. If you use an insulin pump, have insulin pens or syringes on hand in case of a pump failure.
How to Manage Diabetes When You’re Sick

Everyone with diabetes should have a game plan on how to manage diabetes when they’re sick.
Here are a few general guidelines:
- Don’t stop taking your insulin, even if you’re not eating anything. In fact, taking small-to-medium amounts of extra insulin throughout the day may be in order to keep your glucose levels in check. The stress of illness causes the body to release hormones that raise glucose which can increase the risk of DKA, especially if insulin doses are missed or not adjusted upward.
- Test your glucose and ketones every 2-3 hours.
- Rest and drink plenty of fluids. If you’re having trouble keeping fluids down, take small sips every 15 minutes or so to avoid dehydration. If your glucose is low, drink things like regular 7-UP or Gatorade, and if your glucose is high, drink fluids like water and sugar-free Gatorade.
- Take Tylenol for a fever and other over-the-counter medicines as necessary. Many OTC cold and flu meds contain sugar, so check labels or ask your pharmacist for sugar-free options.
In general, take all of your regular medications if you aren’t vomiting.
If your symptoms worsen, your breathing becomes difficult, you have extremely high fevers or you cannot hold anything down, you need to seek medical attention.
Frequently Asked Questions
🍖 How are DKA ketones different from ketones that occur in people on the keto diet?
Ketones are chemicals your body makes when it burns fat for fuel – which can happen during fasting or if you’re on a super low-carb diet. This process, called ketosis, is normal and is sometimes done intentionally for weight loss or for other medical conditions. Diabetic ketoacidosis (DKA) is different – it’s a life-threatening condition that happens when your body doesn’t have enough insulin, and ketone levels go very high and turn the blood acidic.
📈 How quickly can you go into DKA when you’re without insulin?
Unchecked ketones can escalate rapidly to DKA, depending on the individual and the situation. For example, if your pump is leaking insulin a little bit (but not completely) you’re still getting some insulin, just not enough. But if you have a clogged infusion line or your pump falls off and you aren’t getting any insulin at all, DKA can happen much faster. You won’t know if you have rising ketones unless you are checking for them.
🤧 Can you prevent DKA if you’re sick?
The best way to prevent DKA when you’re sick is to follow your DKA management plan. Monitor your glucose closely, check for ketones regularly, give yourself insulin as needed (you’ll likely need more than normal), drink fluids, and stay hydrated.
✅ What is the STICH protocol?
STICH is an acronym that was created to help people remember how to treat DKA if they are on an SGLT2 inhibitor:
- STop SGLT2 inhibitor treatment
- Inject insulin
- Consume Carbs
- Hydrate
Following the STICH protocol can help manage early DKA, but it’s not a substitute for professional treatment if the condition progresses. If you can’t hold anything down, you need to go to the ER.
Flu and DKA: Key Takeaways
DKA symptoms can easily be mistaken for the common flu, but the stakes are much higher. DKA can quickly become a life-threatening emergency if you don’t recognize it, test for it, and treat it. That’s why awareness of the overlap in flu and DKA symptoms—and knowing the differences—is so important.
Everyone with type 1 diabetes, and people with type 2 who take insulin or SGLT2 inhibitors, should have a blood ketone meter with unexpired test strips (or urine test strips) at home. Knowing when to check your ketones can make all the difference between safe self-management and an unwanted trip to the ER.
We expect continuous ketone monitoring will be integrated into at least one CGM in the near future, so hopefully soon you’ll have the option to wear a single device that tracks both glucose and ketones in real time. Remember, Don’t Kid Around when it comes to DKA symptoms!
Explore our resource library and video vault for other tips, tools, and guidance on how to take control of your diabetes.
Support for this educational content was provided by Abbott. Abbott is a partner of TCOYD® at the time of publication; however, TCOYD® maintains full editorial control.
The views expressed in this article should not be used as a substitute for professional, individual medical advice. Individual symptoms, situations and circumstances may vary – please discuss with your healthcare provider.

For CKD patients, my endo does not recommend Gatorade due to high potassium which isn’t great for compromised kidneys.
It depends on how far advanced the kidney disease is, but everyone is different and it’s best to go with the recommendation of your healthcare provider.
Excellent presentation. Very helpful. I got close to DKA one time but had been well educated by my endocrinologist. My only request was as ii was reading this, it would he helpful if I could save this article someway. Thank you door everything. Education is the key.
Thanks for your comment, Emily! I’m not sure what type of computer you have, but if you go to the webpage for the article and hit print, you may have the option to save it as a pdf. Hope that helps! 🙂
I was DKA when I was diagnosed by my GP 45ys ago. He said I would live pass the weekend, he drove me to the hospital and gave me small doses of insulin and kept waking me up and take me for a walk, only a few minutes. Without him I would have died at 26ys old now I am 71, I act quickly now like a month ago I woke up and BS was 21 cdn not USA thats way high gave manual injection of insulin but also was passing out my husband carried me to the living room and sat me down. He was ready to call 911 I said no. It was Sunday, the sugar levels came down with lots of insulin phoned my doctor on Monday morning, got a covid test as we didn’t know if flu or covid. It was positive took anti viral meds but all was good. Unlike 2ys old in UK, doctor told mother she had a sore throat 24hrs later dead, she had DKA. Without my doctor 45ys ago I would have died too. Not all doctors are good
So grateful you had a good doctor 45 years ago, and that you know what to do to treat DKA. Education is key. Thank you for sharing your story.
Great information! Thank you!
I see that there are two kinds of meters for checking ketones. One for blood and one for breath. TCOYD, what do you say is best? And is there a particular machine that you would recommend?
I’m a lot more familiar with the blood test and I would stick to that one because I believe it’s more accurate.
How many symptoms are necessary to test for DKA? Despite several symptoms in the hospital, the providers refused to test me for DKA. Symptoms included: stroke, the providers continually ran my blood sugars high: 200-350+, body aches, lots of fatigue and some brain fog. There was a lot of stress. They said that because I wasn’t vomiting, I couldn’t possibly have DKA. In my assessment, based on this article, it sounds like a DKA test should have been completed. Thank you for this article!!!
You are right in that you don’t have to be vomiting to be in DKA – that’s sort of the end stage. Most cases of DKA have very high blood sugars due to no insulin being around, which causes muscle aches, fatigue, thirst, nausea, and eventually vomiting. And you can have a stroke or a heart attack while in DKA. But there’s no certain number of symptoms, as DKA can be a continuum.
Thank You Master Endo Steve Kenobi! I’ll copy your article to swashbuckle as a lightsaber to self advocate in the future. In honor of Noda ~ With Much Appreciation!!!!
Haha..thanks Anne!
My DKA Dr said I would have died if I didn’t come in when I did. Never had the nausea, vomiting or stomach pain
Old nurse here. There plenty of docs out there who have memorized institution mandated criteria and refuse to deviate – in many cases because the lower the number of tests they order, the higher their bonus. I owe my life to an ER physician who did a CT for bloody urine and found bladder cancer. There are still some good ones out there.
Thanks so much for your comment, and grateful you had a good ER doc to help find the cancer. Hope you are doing well now, and thank you for all your work as a nurse!💛