- Peripheral artery disease is a common vascular condition that occurs when your arteries become narrowed or blocked from too much plaque buildup.
- People with diabetes are at a higher risk for the condition, but PAD often goes unnoticed in early stages because symptoms can be mild or non-existent.
- If left untreated, PAD can lead to pain, numbness, infections, and in severe cases, amputation.
- Anyone living with type 1 or type 2 diabetes should be screened for PAD regularly.
- Lifestyle modifications, medications, and certain medical procedures are extremely successful in slowing the progression of the condition, especially when started early.
Reading Time: 4 minutes
If your legs could talk, they might tell you to stop scrolling TikTok while you’re walking down the street and pay more attention to how they’re feeling. Why? There’s a condition called peripheral artery disease (PAD) that often flies under the radar for a lot of people with diabetes, quietly slowing blood flow to the legs, feet, arms, or hands. Since PAD is asymptomatic at first, it’s easy to ignore…until it’s not.
The good news is that PAD is very treatable when it’s caught early. The bad news is that when it’s caught late, it can lead to serious complications such as amputation, and it can put you at greater risk for heart attack and stroke. Knowing the signs to look for and when to see your doctor can make a huge difference in managing PAD successfully.
What Is Peripheral Artery Disease?
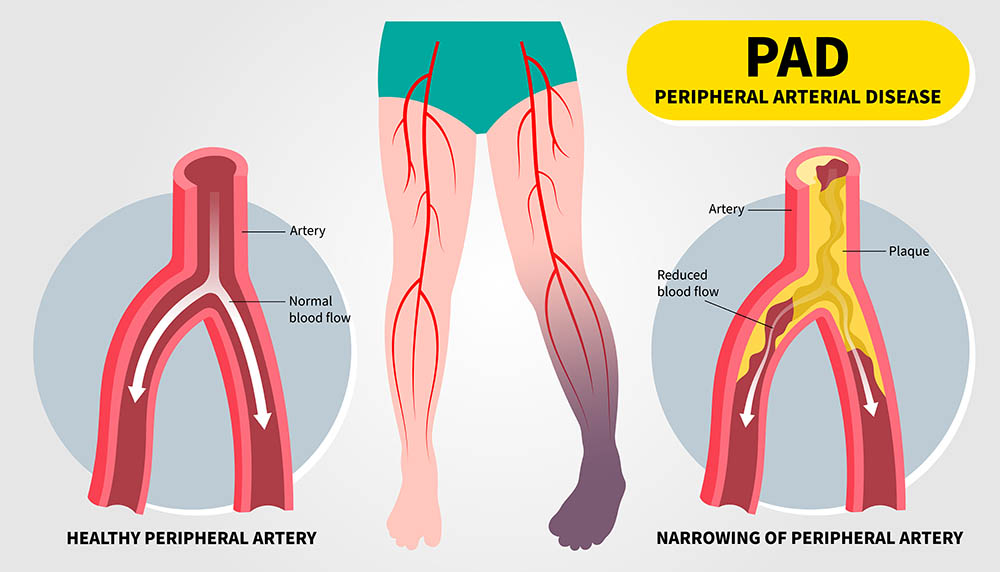
PAD is a vascular condition that happens when arteries carrying blood to your legs, pelvic area, or arms become narrowed or blocked, typically from plaque buildup. Plaque is made up of cholesterol, fats, and inflammatory materials that stick to artery walls over time.
Your arteries are like little traffic tunnels, moving blood loaded with oxygen from your heart to other parts of your body. When plaque builds up on the artery walls (this is called atherosclerosis), it narrows the tunnel and makes it harder for blood to get where it needs to go.
The majority of people with PAD develop it in their lower extremities (hips, legs, and feet). Upper-extremity PAD affects the shoulders, arms, hands, and fingers, but it is much less common and only occurs in about 10% of cases.
Lifestyle modifications, medications, and certain medical procedures are extremely successful in slowing the progression of the condition, especially when started early. The scary part of PAD is that if it’s left untreated, it can lead to pain, numbness, infections, and in severe cases, amputation. That’s why early detection matters – a lot.
Who’s at Risk for PAD?

For a condition that doesn’t get a lot of media buzz, PAD is more common than most people realize. It affects more than 200 million people around the world. Nearly half of Americans between the ages of 45 and 84 are walking around with atherosclerosis and don’t even know it!
You’re at higher risk for PAD if you have:
- Diabetes
- A personal or family history of PAD, heart disease, or stroke
- A history of smoking or tobacco use (past or present)
- Chronic kidney disease
- High blood pressure and/or high cholesterol
- Obesity or low physical activity
- A diet high in saturated fats
- Chronic stress
- Certain non-modifiable factors like race (Black people are at higher risk) or age (if you’re over 65, or over 50 with risk factors for atherosclerosis)
If you have any risk factors for PAD (hello…diabetes), you should talk to your doctor about getting screened because getting ahead of PAD means getting ahead of complications.
What’s the Link between PAD and Diabetes?
PAD and diabetes often influence each other. Chronically high blood sugar from diabetes can damage blood vessels over time, causing arteries to narrow and become more prone to plaque buildup.
Diabetes often travels alongside other artery-stressing conditions like high blood pressure, high LDL (“bad”) cholesterol, high triglycerides, obesity, and kidney disease. Nerve damage (neuropathy) can also complicate things by dulling pain, which may delay recognition of early PAD symptoms.
PAD can make it harder for cuts or sores on the feet to heal, and it can also increase the risk for heart attacks and strokes. That’s why recognizing PAD early and talking with your healthcare provider about screening is so important.
Did we mention that screening is important??
Symptoms of PAD: Silent, Subtle, Then In Your Face!
Not everyone with PAD feels symptoms, especially early on. When symptoms do show up, they’re often brushed off as arthritis, aging aches and pains, or being out of shape.
The first noticeable symptom is often leg pain while you’re walking or exercising that goes away with rest, but then comes back when you start moving again.
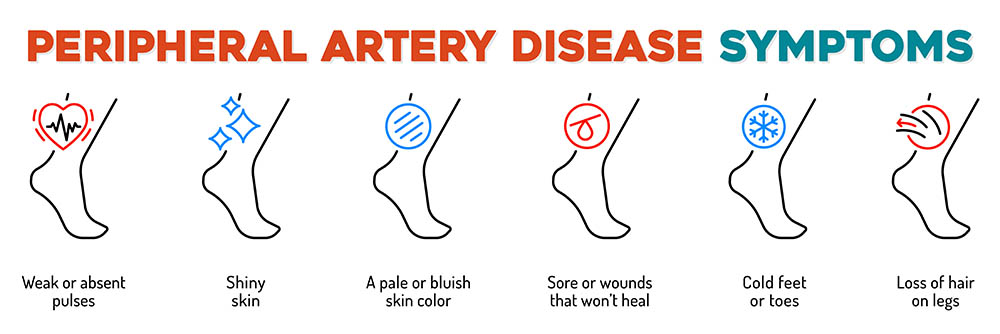
Common PAD Symptoms Include:
- Pain, cramping, or aching in the legs, hips, or buttocks with activity
- Leg numbness or weakness
- Weak or absent pulses in the feet or ankles
- Cuts or sores on the feet or toes that heal slowly (or not at all)
- Slow-growing toenails
- Hair loss or slower hair growth on the legs
- Cooler skin temperature in one leg or foot
- Skin color changes when the affected leg is elevated (skin turns white when the leg is elevated)
- Erectile dysfunction
For upper-extremity PAD, symptoms may include discomfort, pain, tightness, heaviness, or cramping in the arms or hands during use (even with simple movements like washing your hair), hair loss on the arms, swelling, and slow nail growth.
People with diabetes and PAD often develop symptoms that are more serious and progress faster than in people without diabetes, leading to slower or non-healing wounds, infections, and, in severe cases, an increased risk of limb loss.
Because nerve damage (neuropathy) can mask pain signals, many people with diabetes don’t experience classic PAD symptoms. That’s why regular foot checks and PAD screenings are so important for people with diabetes.
The Four Stages of PAD
The rate of progression varies from person to person, but there are four main stages of PAD:
Stage 1: Asymptomatic
Plaque is building up in your arteries, but you don’t feel anything yet.
Stage 2: Claudication
Your arteries have begun to significantly narrow and harden, and symptoms have started to kick in. Leg pain shows up when you walk or exercise, but eases with rest.
Stage 3: Critical Limb Ischemia
Severe blockages lead to pain even when you’re resting, and discomfort is often felt throughout the night. Since blood hasn’t been flowing properly to your extremities to aid with healing, sores and ulcers may begin to appear.
Stage 4: Acute Limb Ischemia
This is a major medical emergency. Blood flow to the limb has suddenly decreased, causing severe pain and tissue damage. Other symptoms include slow pulse, numbness or tingling, coldness, pale skin, and potential paralysis. There’s a very high likelihood of amputation without immediate care.
How Is Peripheral Artery Disease Diagnosed?
Your healthcare provider will begin with a simple physical exam. They’ll check your pulse, examine your feet, and ask about your symptoms. If PAD is suspected, they’ll perform specific tests to see how well your blood is flowing.
Common tests include:
- An ankle-brachial index (ABI), which compares blood pressure in your ankle to your arm
- An ultrasound, which measures blood flow through the arteries
- A CT angiogram, which uses dye and CT imaging to visualize blood vessels
- A magnetic resonance angiography (MRA), which offers cross-sectional images without X-rays
Treatment and Management of PAD
While PAD isn’t curable, it can be slowed and symptoms can improve with early and consistent management. For people with diabetes, managing blood sugar, blood pressure, and cholesterol is especially important.
For many people, lifestyle changes and medications are enough to manage PAD, but others may need medical procedures or surgery.
Lifestyle Modifications:
- Quit smoking
- Get regular exercise
- Control blood sugar
- Follow a heart-healthy diet
- Keep blood pressure and cholesterol in check
- Check feet daily for cuts or sores, wear well-fitting shoes, and avoid walking barefoot (even indoors)
Medication Options:
- Antiplatelet or blood-thinning medications to lower your risk of blood clots
- Statins to help lower LDL (“bad”) cholesterol and slow plaque buildup
- Blood pressure medications to reduce strain on blood vessels
- Vasodilators to help your arteries open up better so blood can flow through
Procedures and Surgical Options:
- Angioplasty and stenting: A catheter is inserted into the artery to open the blockage, and a small stent is placed to keep it open
- Atherectomy: A provider uses a thin tube to reach the affected artery and remove plaque
- Endarterectomy: Another type of surgical procedure that removes plaque from the artery
- Bypass surgery: In severe cases, a surgeon may create a new route for blood to flow around the blocked artery
- Amputation: A last resort for severe cases when circulation cannot be restored
Frequently Asked Questions
🧐 What’s PVD and How Is It Different Than PAD?
Peripheral vascular disease (PVD) is a broad term referring to any condition that affects the vascular system outside of the heart, which includes the arteries, veins, and lymphatic vessels. PAD is a form of PVD that affects the arteries. People (and even providers) often use the terms interchangeably, but PAD is a specific type of PVD.
🔗 Is there a Connection between PVD and Diabetes?
Diabetes is a risk factor for developing both PVD and PAD. Over time, elevated blood sugar can damage the lining of blood vessels, making them more prone to plaque buildup. Diabetes can also worsen cholesterol levels, influence chronic inflammation, and cause nerve damage, which may mask early symptoms of either condition.
PAD and Diabetes: Key Takeaways
Peripheral artery disease is a common but serious condition that builds slowly, often without symptoms in the early stages. That’s why awareness and early screening matter so much, especially if you have diabetes. If you catch PAD early, you have real power to slow it down.
Knowing your risk, paying attention to symptoms, and getting regular checkups with your healthcare provider can help keep those artery tunnels clear and your blood flowing smoothly without bottlenecks.
Explore our resource library and video vault, and subscribe to our monthly digital newsletter for more tips, tools, and expert guidance on how to take control of your diabetes.
Additional Resources:

Our goal is to protect your personal health information. Please keep your questions general and do not post personal medical information here. If you have a specific question, please email events@tcoyd.org.
Thank you for all the valuable information you share with us! I have been Type 1 for 2.5 years, but do not know very much about what a correction factor is and how to calculate it. I live in Canada, so if you answer this question, can you please use Canadian numbers? We use smaller numbers, where the American ones are much larger. Have a nice day! Ann
Sorry that all of our numbers are in mg/dL! To determine your glucose numbers in mmol/L, you would divide the glucose that’s in mg/dL by 18. Here are two articles we’ve done that discuss correction factor, but it will probably be easiest if you find information that’s already in mmol/L, like the first link below:
https://diabeteseducatorscalgary.ca/medications/insulin/insulin-sensitivity-factor-isf.html
https://tcoyd.org/2021/05/how-do-i-know-how-much-insulin-to-take-with-each-meal/
https://tcoyd.org/2020/04/covid-19-diabetes-a-great-time-to-evaluate-your-diabetes-regimen-at-home/