
Prior to 1995, there was only one type of oral medication for people with type 2 diabetes: the sulfonylureas (SFUs). This meant that people with type 2 diabetes had the option of SFUs or insulin, or both, to control their blood glucose levels. Sulfonylureas lose their effectiveness over time, and since no one likes to take injections and it was easier for the healthcare providers (HCPs) to prescribe pills instead of an insulin regimen, many people with type 2 diabetes lived with poor glucose control for several years. Commonly, it was only when the blood glucose level became extremely high, into the 300- to 400-mg/dL range, that insulin therapy had to be initiated to finally bring down the toxic levels.
With the advent of multiple new oral medications, this situation is improving, but we still have a long way to go. The progress has been painstakingly slow because some HCPs do not know about the advances made in this area, and much of the public is unaware as well, which is why patient education, motivation, and activation are so important. The bottom line is that if you have type 2 diabetes, you need to know what new therapeutic advances have been made and are available right now. If you think that any of the medications you read about in this series may be good for you, please discuss it with your HCP.
We now have lots of choices!
Since 1995, several new types of oral and injectable medications for people with type 2 diabetes have become available, with many more under development. These diabetes drugs can be given together and/or with insulin to more effectively control the glucose level throughout the day and night. Since many of these oral agents have not been on the market for an extended period of time, it is of utmost importance that you become knowledgeable about all of them, and determine if one or more of them would be helpful to you. Oral diabetes medications and the incretins are generally not approved by the FDA for people with type 1 diabetes or for women who are pregnant and/or are breastfeeding.
There are now nine major classes or types of oral medications for people with type 2 diabetes.
This month we’re going to talk about Sulfonylureas. Sulfonylureas, or SFUs, have been around for a long time. For decades, these were the only oral medications available for people with type 2 diabetes. They were the workhorses of the 70s, 80s, and early 90s. There are many different SFUs on the market today, and they all work primarily by stimulating the pancreas to secrete more insulin.
Even though the tissues of the body are resistant to the glucose-lowering effects of insulin, if the insulin level becomes high enough in the blood from taking SFUs, the glucose levels will eventually start to fall. Most SFUs on the market are listed in Table 7-1, along with the recommended dosage range, including how often they should be taken per day (depending on the duration of action or how long they hang around in the body).
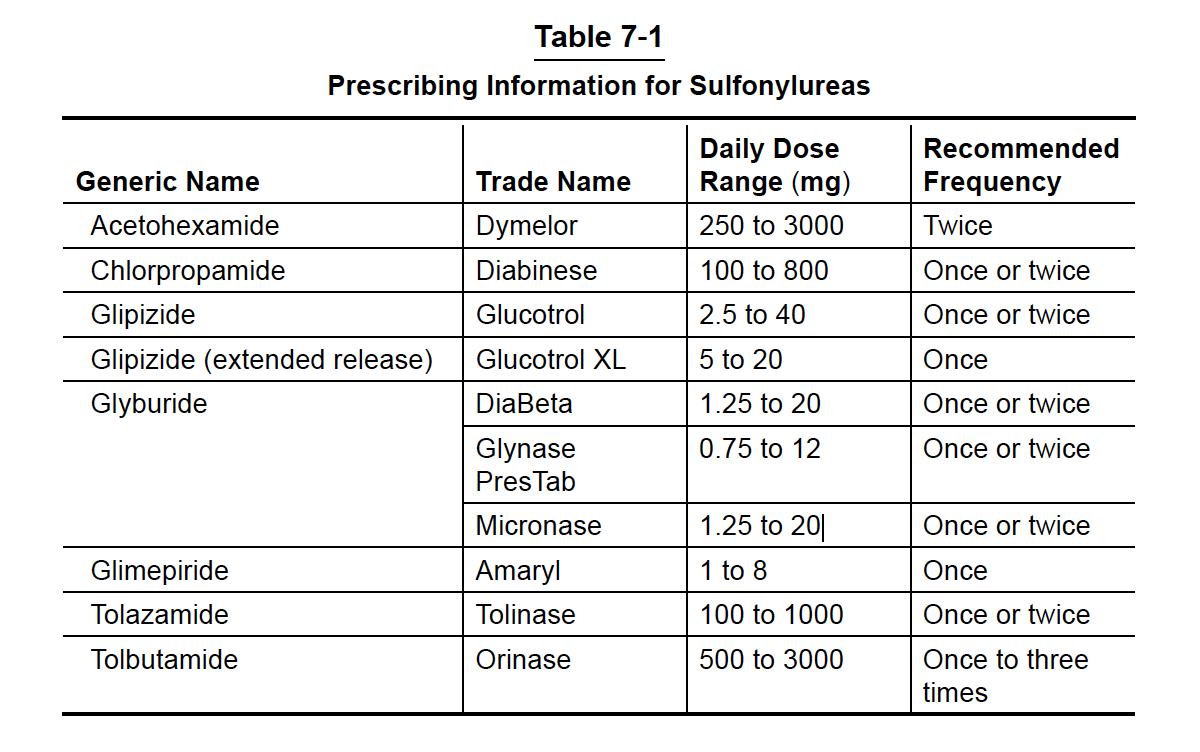
Some of the longer-acting SFUs, such as Diabinese (chlorpropamide) and Diabeta (glyburide), require extra caution, especially if you are elderly (older than me) because they tend to stay in your system for a longer period of time (up to 3 days for Diabinese) and can therefore increase the risk of hypoglycemia. For example, if you become ill and cannot eat, you will have the tendency to have low blood glucose for a prolonged period of time despite stopping these medications.
The pros of SFUs
SFUs are effective in bringing down the blood glucose values and are generally well tolerated (do not have a lot of side effects) by people with type 2 diabetes. They are also one of the least expensive oral diabetes medications. The combination of a cheap and effective diabetes drug makes SFUs a good choice for many patients. However, they do have some shortfalls.
The cons of SFUs
One of the main problems with the SFUs is that they lose effectiveness over time, on average after about 5-10 years of use; however, the response is different from individual to individual. The results of ADOPT (A Diabetes Outcome Progression Trial) published over 10 years ago clearly demonstrated that SFUs fail to maintain control over time compared with other oral medications such as metformin and rosiglitazone (Figure 7-1).
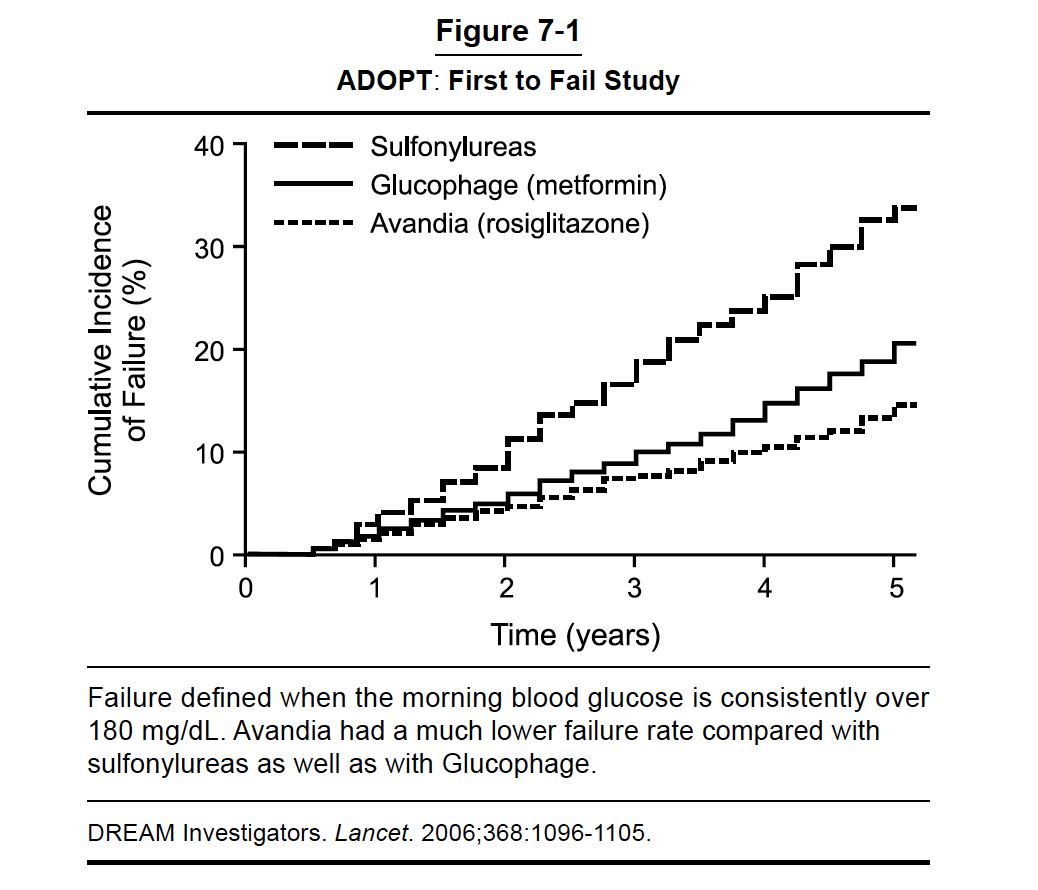
Some researchers believe it is because the SFUs work by making the pancreas work overtime, eventually leading to exhaustion and reduced insulin secretory capacity over time. If the pancreas is exhausted, it cannot put out any more insulin, and you will not be responsive to SFUs anymore. Thus blood glucose goes out of control. When a person’s glucose values start to rise while being treated with an SFU, it is usually necessary to add another oral medication or initiate an incretin agent or insulin therapy to get the diabetes under control. When this happens, your HCP will determine if the SFU should be discontinued.
A second shortfall is that SFUs commonly cause 5 to 10 pounds of weight gain, most likely because of the way they work. When insulin levels go up, either due to insulin secretagogues or insulin injections, the body weight also has a tendency to go up.
A third shortfall is that SFUs can cause low blood glucose (hypoglycemia), especially after strenuous exercise, if you miss a meal, or if you lose weight. Sometimes patients need to hold their SFU medication for a few days if they are not eating (for example, with a severe illness.) Once you start eating regularly again, you should restart the SFU. However, it must be remembered that hypoglycemia is not a severe problem in the majority of cases and is normally recognized early and easily treated. If you are a person whose diabetes has been recently diagnosed (less than a few years ago) or if you have normal or near normal blood glucose levels, you might be at a higher risk for hypoglycemia on SFUs than someone who has had diabetes much longer with poor control.
Keeping an eye out for hypoglycemia
The main symptoms of hypoglycemia are shaking, sweating, palpitations (feeling your heart beating over your chest area), and confusion. If you think your blood glucose is getting too low, you should drink or eat something sweet, such as 4 to 8 ounces of fruit juice, regular soda, four to six Lifesavers, or one of the many forms of glucose tablets that are sold over the counter (without a prescription) in pharmacies. You should always carry something sweet, such as a pocket-sized container of glucose tablets, and keep similar items in your car, at your place of work, and/or at school. It may also be important to tell your family members and coworkers about the signs of hypoglycemia and how to help you (if necessary) during a low blood glucose episode.
When you think you are experiencing hypoglycemia, if possible, try to test your blood glucose level before treating yourself with sugar to make sure that your symptoms are in fact due to hypoglycemia. This helps you and your HCP know when you have actual episodes of hypoglycemia and to properly adjust your medication. You should call your doctor if you have low blood glucose episodes frequently, especially if it happens without a ready explanation (such as a missed meal or during strenuous activity).
In next month’s newsletter, we will discuss another of the many different oral medications to treat type 2 – biguanides (metformin).


Thank you. I am interested in the new prickles test. Please report on it soon. We need to bring the Patrice down.
Thank you for all your information on the first group of medications (sulfonylureas) for Type II diabetics. I found this very helpful in increasing my understanding. Is there any way I can personally get the information on the other 6 groups before you are scheduled to include them in the newsletter? I will be going to my PCP on 11/5 to discuss a probable change in medication and I would like to be more informed. I attended your conference in St. Louis and thank you for all that you do beyond treating your individual patients.
Hi Carol,
Yes absolutely! The medication breakdowns are all in Dr. Edelman’s Taking Control of Your Diabetes book, in a little more detail. There are hard copies and digital copies of the book available and both are $20. (If you order the hard copy, there is a shipping fee of $7.25) Feel free to call our office at 800-998-2693 if you would like to order one. Take care!
i am interested in neuropathy which is not mentioned any where. my legs are now numb up to my knees and nothing is done about it except taking neurontin which leave me sleeping. Lipoic acid does not seem to do anything either. we do not have a neuropathy center here in Lompoc ca like they do in Huntsville Al. where they are trying things that seem to work .
i guess i need to move there for some help. Thoroughly disgusted with the Diabetic people who never mention it.
When i was diagnosed the office girl called me to pick up the medication at the pharmacy. The Doctor never explained anything to me. i am lucky i knew about it as my Mother had it. I lost my MOther when i was 47 now is am 87 and have had Diabetes for 17 years.All 4 of my sons are complaining about feet aching. That is how i started and was told to get Spenco inserts at Big Five store. How stupid is that with a Life threatening disease and from a Doctor at that.
I was a Nursing Asist which also helped me.i had a friend who had bad breath and i told her to get a glucose test. She was Diabetic and didn’t know it.
Hi Lucille,
There is a chapter in Dr. Edelman’s book that goes into great detail about neuropathy. The book (in digital or print form) is $20 (plus shipping for the print version). If you would like to order the book, you can call our office at 800-998-2693 and anyone who answers the phone can help you. It sounds like you may want to also consider changing doctors (or getting another opinion) if you feel your current physician isn’t providing the care or education you would like. Also just so you know, we are holding a conference in Santa Clara on March 30th if that is not too far away for you.
I currently take Metformin ER 750 mg and Januvia 100 mg. I recently was told to cut my Januvia 100 mg down by the pharmacist when I went to refill it last week.
The pharmacist cut my dose in half for the Januvia 100 mg. When I called and asked he said one of the blood test back in July was off. I contact MD office and so far no reply.
Hi Sharon,
Obviously you need to speak to your doctor, but the dose of Januvia needs to be adjusted based on kidney function. Every situation is different, so give him/her a call back.
I have problems with hypoglycemia when my Blood Sugar is normal; however, I feel great when my Blood Sugar is high. Any comments Doctor? This has been going on for years; I prefer not to have the hypoglycemia episodes.
What you’re experiencing is normal. Typically you should slowly try to edge your glucose values in the normal ranges, and the key is slowly. Also get an Abbott Libre so you can get a blood glucose value any time you want to give yourself confidence of avoiding a low.