
Reading Time: 5 minutes
This case is important to highlight for the following reasons:
- Hypoglycemia is classified into different levels with specific symptoms. Understanding these levels is key to recognizing when low blood sugar is mild or severe so it can be treated appropriately.
- Everyone should be aware that glucagon can be self-administered; it does not require administration by another person. Early use is acceptable and can help prevent progression to a severe stage.
In the not-too-distant past, self-administration of emergency glucagon was blasphemy!
Emergency glucagon was only reserved for someone who was so hypoglycemic they were doing the fried egg (having a seizure) and could not help themselves.
With the advent of newer glucagon emergency kits that are easy to administer, people with diabetes who use insulin discovered that self-administration of emergency glucagon could be a lifesaver. It can help prevent altered consciousness, seizures, and potential death from a severe hypoglycemic reaction.
The Patients: Dr. E & Dr. P
As many of you know, both Jeremy and I were diagnosed with T1D at the age of 15…only 25 years apart!
We both struggle to keep our time in range (TIR) above 70% while limiting hypoglycemia. Despite the development of continuous glucose monitors (CGM), physiologic designer insulins, and hybrid closed-loop systems with automatic insulin delivery, hypoglycemia is still a consistent problem for us (and the millions of folks living with diabetes on insulin).
Jeremy’s Hypoglycemia Tale: Injecting the Wrong Insulin
A few years ago, Jeremy took a break from his insulin pump and switched to multiple daily injections because he just wanted to be untethered from his pump for a while. He still wore his CGM because that is one device you do not want to take off!
He was taking 35 units of long-acting basal insulin per day, and 5 to 15 units of fast-acting insulin before each meal (depending on his glucose level, trend arrows, and planned carbohydrate intake).
One night Jeremy got his insulin pens mixed up (they looked very similar), and he gave himself 35 units of fast-acting insulin instead of 35 units of basal insulin. This happened at bedtime when his glucose level was 126 mg/dL with a horizontal trend arrow….YIKES!!!
He started to feel hypoglycemic so he had several glucose tabs, but his glucose level continued to drop. He was in a hotel room in Boston, and he called me in San Diego when he realized his mistake.
We decided he should administer the emergency glucagon he had packed in his suitcase. THANK GAWD he packed it!
Jeremy’s glucose value was 47 mg/dL and dropping.

He had already eaten every glucose tab and snack he had, and he had raided the minibar. Even if he had more food to eat, he said he could not eat another thing as he was stuffed to the gills. His symptoms of hypoglycemia included tremors and palpitations, and he was sweating and feeling very weak.
Jeremy’s glucose level reversed direction and reached 205 mg/dL 30 minutes after the glucagon injection. He did fine overnight, but he set his alarm to wake up every hour to check his numbers.
It’s a scary scenario to have severe hypoglycemia in a hotel room by yourself. Having an unexpired glucagon emergency kit is a must for anyone on insulin and/or sulfonylureas, and self-administration can be a lifesaver.
Steve’s Hypoglycemia Tale: A Diabetes Technology Malfunction
My tale is not too different from Jeremy’s. I was on my normally very reliable hybrid closed-loop (HCL) system while traveling to D.C. for a speaking engagement. My CGM had been acting up – it was skipping readings and the trend arrows weren’t showing up.
When I was getting ready for bed in my hotel room I started to feel low. My CGM said I was 187 mg/dL, but when I checked my glucose meter it was 63 mg/dL!

My HCL system had been giving me quite a bit of insulin in response to the glucose value that was incorrectly high. Although I suspended insulin delivery, it was too late because the insulin had already been infused and was causing me to drop.
Like Jeremy, I ate all my glucose tabs and snacks, but I was still dropping and I could not eat another thing. Since I have gastroparesis, the food was sitting in my distended stomach not being absorbed, which would have helped to raise my glucose value.
I immediately injected my emergency glucagon, and within 10-15 minutes my glucose did a 180-degree turn and was trending upward.
My girlfriend Jamie follows my glucose values and was alerted when I got below 55 mg/dL. She called to check on me and was irked because I had not texted her earlier with the phone number of the hotel and my room number – a good safety measure in case I did not answer her text or call.
After 45 minutes my blood sugars were stable and I was able to “try” to go to bed. I say “try” because I slept restlessly through the night.
I was very thankful I had my emergency glucagon kit with me. The next day I went to a local CVS and picked up a new emergency glucagon kit because I was staying in D.C. for another night and I didn’t want to be without one.
The Solution: Be Prepared for Hypoglycemia
These situations are more common than you think. Technology can malfunction and people can make mistakes.
It’s important to know that you can self-administer emergency glucagon to prevent a severe hypoglycemic event – you don’t have to wait until you’re in one and unable to help yourself!
There are three general hypoglycemia levels:
- Level 1: Mild hypoglycemia: blood glucose is less than 70 mg/dL
- Level 2: Moderate hypoglycemia: blood glucose is less than 54 mg/dL
- Level 3: Severe hypoglycemia: no specific glucose value – a person is unable to function because of mental or physical changes due to low blood glucose
Level 1 is typically managed with fast-acting carbs. Intervention with glucagon may be necessary at level 2.
If you wear a continuous glucose monitor, trend arrows are key to understanding how quickly glucose levels are changing – especially when they’re dropping.
It’s also important to remember that symptoms of low blood sugar can vary from person to person—some people may not feel low until their glucose reaches 65 mg/dL, while others may start experiencing symptoms around 75 mg/dL.
What Are Common Symptoms of Hypoglycemia?
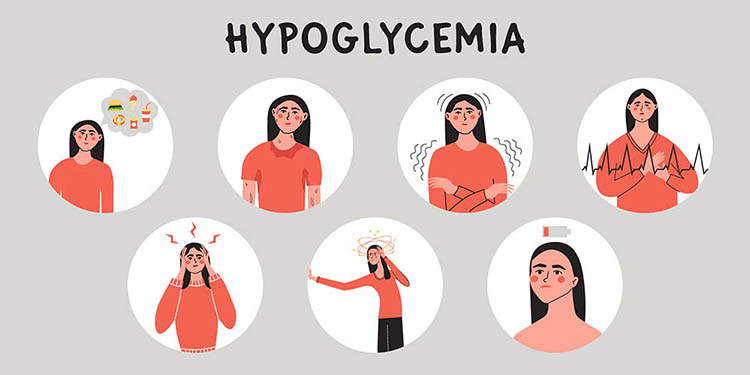
Mild symptoms of hypoglycemia (also referred to as adrenergic symptoms) as blood sugar starts to drop below 70 mg/dL include:
- Hunger
- Sweatiness
- Trembling or shaking
- Heart palpitations
Severe signs of hypoglycemia (also called neuroglycopenia) include:
- Headaches
- Lightheadedness and dizziness
- Confusion
- Difficulty speaking
- Seizure
How to Be Prepared for Hypoglycemia
If you take insulin and/or sulfonylureas such as glipizide (Glucotrol) or glimepiride (Amaryl), the following steps can help you stay prepared for hypoglycemia:
- Carry a glucose meter to confirm hypoglycemia symptoms, and/or to confirm your blood sugar if your CGM value does not match how you feel
- Keep plenty of fast-acting carbohydrates on hand (at home, at work, in your car, in your gym bag, etc)
- Keep unexpired emergency glucagon on hand and know how to use it
If you are wearing a CGM, it’s a good idea to have a friend or loved one follow your glucose values.
Key Takeaways
There are many reasons for hypoglycemia. The best thing you can do is be as prepared as possible in case it does occur.
Everyone with type 1 diabetes, and those with type 2 diabetes who are on insulin or sulfonylureas, should have a glucagon emergency kit. Tell your family, friends, and coworkers where you keep your emergency glucagon and explain how to use it.
You don’t have to wait for severe hypoglycemia before using your emergency glucagon. If you’re going low and your trend arrows are pointing downward, you can intervene before a severe hypoglycemia event.
Many people do not think they need an emergency glucagon kit…until they need one!
Hopefully, this knowledge will help you feel more in control and less fearful of lows. Visit our resource library and video vault for more information on living well with diabetes.
Self-administration of emergency glucagon is a safe and effective way to prevent a seizure or visit to the emergency room …or worse!
Editor’s Note: Xeris Pharmaceuticals® is an active partner of Taking Control of Your Diabetes® at the time of publication. TCOYD® maintains control over editorial content. Please consult your healthcare team before making any changes to your diabetes care regimen.
Additional Resources:

Baqsimi is an inhaled glucagon that is very simple to administer. Do you have any cons on Baqsimi?
Some people complain that they had headaches afterwards, and felt like they got hit in the head by a car airbag.
Medicare doesn’t pay for Glucagon. And post-deductible copay is $250. Mind-blowing…
That’s awful. Medicare is very complex and there are so many different plans and coverage options. Medicare does pay for the older version that you have to mix, though that’s not idea. If you haven’t already, you might consider seeing a Medicare SHIP counselor in your area – they are volunteers who can help people find the best plan for their needs and situation. You might also try calling the companies who make glucagon to see if they have patient assistance programs. You might also see if there are any free clinics in your area that have glucagon, or see if your doctor has any samples.
That is why I won’t use it. The one and only time I had it, it expired and all that money gone.
Hopefully things will change in the not too distant future. 🤞
My Medicare does pay for Glucagon!!!
Oh that’s GREAT!!
I’ve been carrying a Glucagon kit for the past year or so. My sugar regularly drops below 54 at night (into the 30s a couple of times). My doctor didn’t think any type 2 diabetic needs Glucagon, although I asked for it twice. Another endocrinologist who was covering for him over a holiday prescribed the Glucagon after one of those nights of readings in the 30s.
If you have type 2 diabetes and you’re on insulin or a sulfonylurea (like glipizide, glypuride, amaryl), you should have an emergency glucagon kit because both of those drugs can lower your blood sugar. There’s no question about it. The incidence of lows is not as high as in type 1s, but it’s still there.
I do have Bagsimi and thankfully, I have never had to use it yet. With a glucagon pen, can’t you administer in smaller doses versus the Bagsimi? Would a glucagon pen also be helpful so you don’t go sky high after administering it and not have the headaches as I have read?
Hi Carol,
Dr. Edelman is traveling at the moment, but he suggested you check out this video and podcast which go into more detail about mini dosing glucagon:
https://tcoyd.org/2024/03/updates-in-glucagon-including-mini-dosing/
https://tcoydthepodcast.transistor.fm/48
Hope that helps!