My patient Alan is an 84-year-old retired physician with a long history of type 2 diabetes and chronic kidney disease. He’s been taking 10mg of Farxiga once a day. Farxiga is a medication used to help improve blood sugar control, and it also helps protect against worsening heart failure and chronic kidney disease. Alan also takes long-acting insulin Lantus at night.
Alan’s fasting glucose levels first thing in the morning have been pretty adequate – generally in the 130 to 160mg/dL range. However, his A1c at his last appointment was 7.9%.
I ordered a FreeStyle Libre continuous glucose monitor for him to wear so I could determine why his A1c was high, despite his good blood sugar levels in the morning.
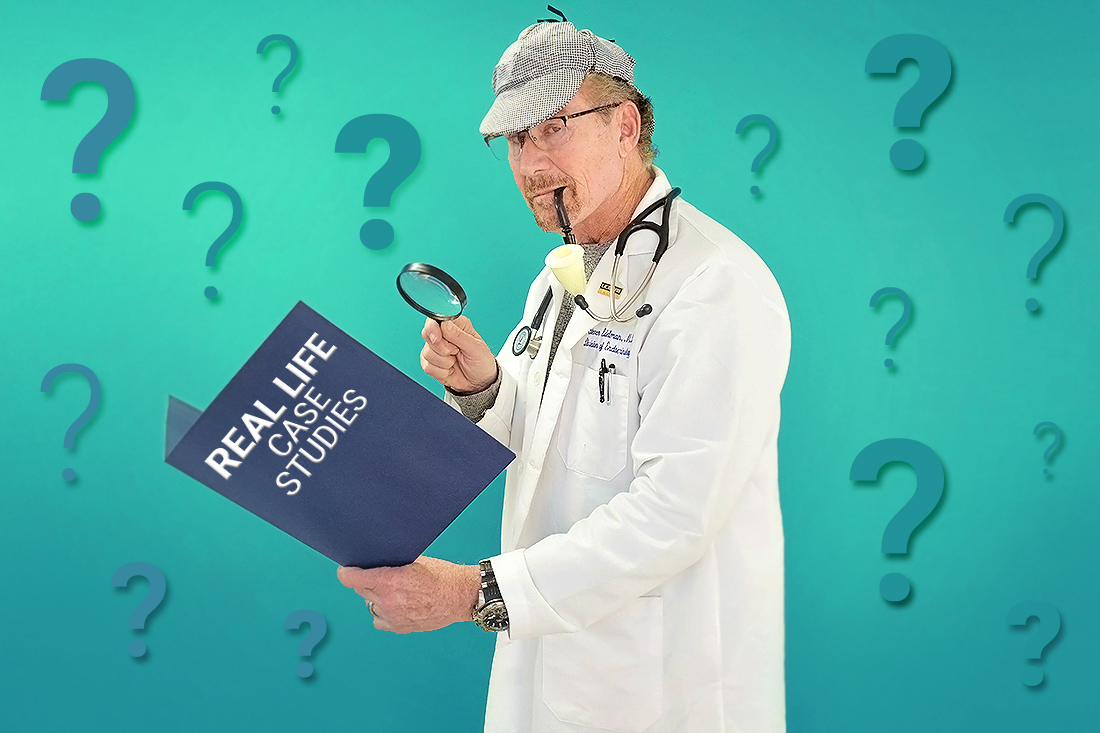
After wearing the CGM for several weeks, I examined his data (below) and could see that his blood glucose levels went through the roof after his dinnertime meal.
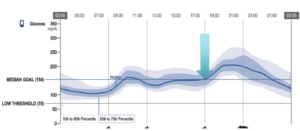
I added one shot of fast-acting insulin Fiasp* to his regimen at dinnertime, and I titrated it up to 15 units of Fiasp 20 minutes before dinner. As you can see from the second CGM download below, this totally took care of the problem.
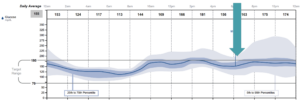
In the CGM report below, you can see that Alan’s A1c came down to 7% with no hypoglycemia. In a CGM report, the Glucose Management Indicator (GMI) is the average blood sugar over the past three months and is equivalent to an A1c (and generally more accurate). His time in range went up to 77%, well above goal!
Thanks to Alan’s CGM data, I was able to determine what the most critical problem area was, and we were able to address it. Taking one shot of a rapid-acting insulin with a single meal is not uncommon for someone with type 2 diabetes, and remember that when you take your mealtime insulin is extremely important!
This case is a perfect example of the benefits of using a continuous glucose monitor to pinpoint the cause of an elevated A1c, and how instituting a targeted therapy can really make a difference.
*Although I prescribed Fiasp for Alan’s mealtime insulin, Novolog, Humalog, Lyumjev or Afrezza could also be used.


I read all the books on insulin when I was diagnosed. The majority of these books covered the history of Diabetes technology and complications. Very little on real world insulin dosing.
These case reports give great examples of what we need to do or change. Please keep them coming! It’s a great education for those of us who are new.
Will do – thanks for the feedback, Jodi!
Thank you so much for that report. I am 82 and have the same problem after my breakfast and dinner. No matter how much or how little I just can’t do carbs. My A1c is 6.8 and apart from Berberine I don’t take Rx.
Wow. With an A1c of 6.8 you are doing well, especially without diabetes drugs!
This is interesting. My A1c’s are always 5.5-5.6 (sure this is in part to avoiding eating because i will become symptomatic) no matter what. blood work always shows my fasting glucose to be 105-120. so no one even suspected a problem even at my first endo visit he said i was not diabetic. but when i showed him my BGM readings and OGTT test he quickly changed his mind. Just like mentioned i can not eat a carb if i had to without spiking badly. he has since put me on a fast acting insulin and i was able to get a few free CGM’s and the data is very telling and we already made a dosage change (more work to be done yet) Insurance has now approved the libre.
Just to point out that the DM clinic i go to is able to do 2 diagnostic CGM’s for most folks. it’s worth inquiring into.
Glad you were able to get a CGM – they truly are game-changers.