The Patient:
My patient Kathy is a 72-year-old woman who was diagnosed with type 1 diabetes at the age of 40. She wears a Dexcom CGM and is on the Tandem Control-IQ hybrid closed-loop pump.
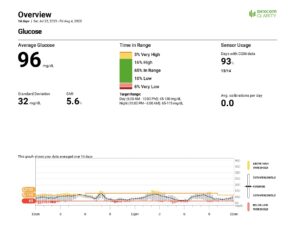
Here’s a snapshot of Kathy’s 14-day Dexcom download:
The Problem:
As you can see from Kathy’s shocking download, she is low (“low” meaning 55 to 70 mg/dL) 10% of the time, and very low (below 55 mg/dL) 6% of the time. One percent represents 15 minutes, so she was below 70 mg/dL 4 hours a day on average for the duration of this download! She was below 55mg/dL for 90 minutes a day on average!
Kathy has always kept her glucose levels very low as she has the misbelief that her A1c needs to be below 6.0%. She has had many severe hypoglycemic reactions requiring paramedic visits and many trips to the emergency department. Her husband tells me she is very stubborn, and he is at his wit’s end. Thank God Kathy is on the Tandem CIQ pump because the suspend feature has kept her alive on multiple occasions. In addition, she tells me she does not feel her lows anymore, making the situation more dangerous.
When I looked at where she had set her alerts and alarms, I was shocked again:
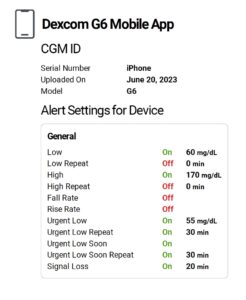
Her low alert was set at 60 mg/dL which is way too low for anyone, but especially for her due to her hypoglycemia unawareness. Her repeat low alarm and rapid fall rate alarm were also turned off. Not smart!
The Solution:
Kathy needs to make a lot of changes, but I can only make suggestions. I talked to her about making the following adjustments:
- Raise her low alert to 90 or 100 mg/dL so she can catch lows as they are happening and react to them before she gets dangerously low.
- Turn on her repeat low alert (which goes off every 15 minutes) and her rapid fall alert.
- Lower her basal rate and raise her sensitivity factor.
I am worried about her and I hope when I see her next she’s made even just one change that will help keep her in a safer spot.
The Takeaway:
This case is a classic example of the misconception that having a low A1c means your control is good. If you were to look at Kathy’s CGM metrics individually, you might think she’s doing well. Her mean glucose is a little low but good, her standard deviation is excellent, her time in range is almost 70% (so close to goal) and she has very few highs. But (and that’s a very big but) when you look at the amount of lows she has, that percentage is shockingly high.
Therapists who specialize in helping people with various aspects of diabetes management like Dr. Bill Polonsky at the Behavioral Diabetes Institute can really help people in these types of situations.
As a doctor, I can only make suggestions and provide information to my patients, and they make their own decisions. But I still hope my patients listen to me!
Additional Resources:
A1c Goals: How Low Should You Go?


This is a serious case of patient blaming if I ever saw one.
Perhaps she’s rightly afraid of the serious long term complications that come along with running high blood sugars.
Why do doctors like you insist on running their patients way higher than normal? An A1c of 6% is nearly 2x normal and will make long term complications much more likely.
Why not help her achieve a truly normal A1c of under 5%? It can be done with the amount of lows cut way back and much smaller SD. We are all entitled to normal non diabetic blood sugars and to live a life free from gruesome complications.
Mike…I get it about avoiding complications, but for a 72-year-old woman with hypoglycemia unawareness, 90 minutes a day on average below 55mg/dL is dangerous. Stay healthy.
Edelman, an A1c under 6.0% is not “low”, in fact even from 5.7-6.0 it is still elevated. An A1c in the mid to low 5s or high 4s is also not “low”, but normal and non-diabetic. Diabetics deserve to have normal and non-diabetic blood sugars and A1c.
Dr. Attar, I understand the issue of avoiding complications, but for a 72-year-old woman with hypoglycemia unawareness, 90 minutes a day on average below 55mg/dL is extremely dangerous. Stay well.
This sounds like exciting research. It’ll be interesting to see if that molecule works both safely and shows a difference; even if it doesn’t, that’ll be something to learn from, too. Good luck to the team!
We’ll pass that on…thanks Jason! 🙂
In general for a T1D patient, what alert levels do you suggest?
I use the Libre3 CGM. I use Treshiba for my basal, and primarily Affrezza for meals. I use Lyumjev for post meal touch up adjustments if needed.
My blood A1c is 5.7 and my CGM estimates my A1c at 6.2. These differences are consistent.
If you do not recognize your lows, then 90 or 100mg/dL for your low alert, but if you do recognize your lows, then 80mg/dL. Just my recommendation. You can also watch our videos that delve into it a little more here:
https://www.youtube.com/watch?v=XQNib93oLZM
https://www.youtube.com/watch?v=wh6d-aWaXAM
Thank you for all the you do, Dr. Edelman! Along with my endocrinologist and diabetes health educator, I consider TCOYD one of my primary sources for learning more about and truly gaining more control over my T1D, please keep it up!
Thanks Maryam…very kind of you.
I think this case study is a great argument for why focusing on A1C (at any level), without also focusing on Time in Range is seriously misguided. I also prefer to keep my A1C below 6 to most effectively avoid long term complications, but I work very hard (with help from Control IQ) to make sure I’m doing so safely (A1C = 5.5, TIR = 96%, 2% low, <1% very low). That's a whole different ballgame than Kathy in the example. Kathy needs to focus on getting those lows under control for sure.
Absolutely…time in range is so important. Great job on yours! 🙂
I find myself wondering if Kathy has a glycation gap, and if that might be playing into things. I have never (personally) been able to achieve a (lab) A1c below 6.5-7% without a % of time below 70 with which neither I nor my endocrinologist are comfortable.
There are lots of people, including me, that just can’t A1cs that low, and we don’t need to.
I think someone like your patient has listened to too many lectures on you tube by Dr. Bernstein. He’s always saying the line diabetics are entitled to non diabetic blood sugars and insisting patients are doing something wrong if they’re A1Cs are over the mid 5s.
I think he’s frightening a lot of us Type1s who have the free time to watch his lectures.
I was finally able to be happy and relaxed with my 6.1 A1C after finding TCOYDs videos on the subject. I’m content to know that I don’t need to struggle to get it any lower. This allows me to eat a moderate carb lower saturated fat diet which is what I like and has lowered my LDL to what you and Dr. Pettus recommended.
Thank You!!!
Thank you so much for your note. I totally agree with you!