
I’ve been a type 1 diabetic (T1D) for 23 years, and I’m also a pharmacist. I control my blood sugar by using an insulin pump and continuous glucose monitor (CGM), and I cannot stress how beneficial having a CGM has been for helping me understand my blood glucose (BG) trends with various foods and activities.
I discovered CrossFit in 2013, and I quickly became hooked on the community-oriented, high intensity, constantly-varied method of endurance and strength training. However, with a unique Workout of the Day (WOD) every day, it became frustrating to see my BG drop too low during or after my workout since we all know that hypoglycemia can be such a thief of joy!
What Is CrossFit?
CrossFit is made up of both aerobic exercise, which is the sustained steady state heart rate (HR) of 55-80% of one’s max HR, and anaerobic exercise, which is 80-90% of one’s max HR that can be sustained for no longer than 90 seconds to 2 minutes.
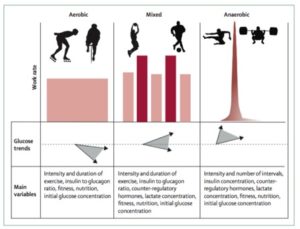
Aerobic Exercise and Insulin Sensitivity
When performing aerobic exercise (e.g. running), muscles become more sensitive to insulin, which promotes increased glucose uptake by the cells. As a result, insulin levels drop to allow the liver to produce glucose. However, in T1Ds, insulin levels are almost always too high to allow the liver to produce enough glucose during exercise to replace the glucose being taken up by the muscles for energy.
Stress hormones like adrenaline and cortisol, which normally raise BG and counteract high insulin levels, are reduced during exercise, further decreasing the body’s glucose supply. Without taking any action, these factors often result in hypoglycemia!
Anaerobic Exercise and Insulin Sensitivity
Alternatively, anaerobic exercise (e.g. weightlifting) uses less glucose during the activity, and there is a quicker release of stress hormones that signal the liver and other organs to produce glucose. This may have the opposite intended effect and cause BG levels to rise.
Here Are a Few other Pearls I Have Learned along My Fitness Journey:
- The risk of hypoglycemia is elevated for at least 24 hours in recovery from exercise, with the greatest risk of overnight hypoglycemia occurring after afternoon exercise activity because it takes the body 12-24 hours after activity to replenish the glucose storage, a.k.a. glycogen
- Exercise increases your insulin sensitivity factor (ISF), meaning one unit of insulin may have a more significant BG reduction compared to a non-active day. Example: 1 unit of insulin lowers BG by 20 mg/dL (1.1 mmol/L) on a non-active day vs. 1 unit of insulin lowers BG by 40 mg/dl (2.2 mmol/L) on an active day
- CrossFit competitions can cause stress hormone release which can raise BG
- Upper body exercise is more likely to raise BG compared to lower body exercise
More guidelines on exercising with diabetes can be found here.
(Disclaimer: Your diabetes may vary! Treatment methods and the impact of exercise are very individualized, so please talk to your endocrinologist before making basal rate changes on your pump.)
Insulin Dosing Strategies for Exercising (Using an Insulin Pump):
- A basal rate reduction, rather than basal suspension, may be attempted 60-90 minutes before the start of exercise
- An 80% basal rate reduction at the onset of exercise helps mitigate hyperglycemia after exercise more effectively than suspending the pump, and appears to reduce the risk of hypoglycemia both during and after the activity
- Bolus dose reductions require planning in advance and are probably only appropriate for exercise with a predictable intensity performed within 2–3 hours after a meal
- A time limit of less than 2 hours for insulin pump suspension is proposed due to the pharmacokinetics (how the drug moves through our bodies) of rapid-acting insulin
- To minimize overnight hypoglycemia, a 50% reduction of bolus insulin dose is recommended for the meal following exercise
After much trial and error, my “ah-ha” moment arrived when I exercised 2 to 3 hours after a meal (with minimal active insulin on board) and reduced my basal rates by 50% for 90 minutes before my WOD and continued the 50% basal rate reduction throughout the 60-minute workout. This method allowed my BG to remain stable during the workout, but what about those pesky overnight low blood sugars? Even after reducing overnight basal rates following exercise and including a protein snack, my BG would still drop too low, which led to many sleepless nights. To be honest, I never overcame this…until I started looping!
The Looping Game Changer
Dr. Edelman has talked about his own experience looping with Omnipod here, and I’m also on the looping bandwagon but with OpenAPS.
Nowadays, after an afternoon workout, I can sleep through the night even if my blood sugar starts to drop because OpenAPS will suspend my pump until my BG level starts to rise to my target BG range. At the gym, I can also set a temporary BG target to keep me in range when I’m doing a WOD with a lot of cardio like this:
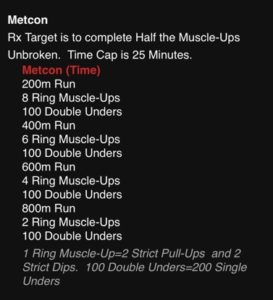
(Note: My gym allows us to see the WOD beforehand and I can plan my diabetes treatment strategy appropriately.)
Occasionally, I will have a slightly higher BG after some WODs with heavy weightlifting, but it’s usually short-lived as OpenAPS will deliver a SMB (super micro boluses) to lower my BG back to my normal range.
Although CrossFit is constantly varied, over time we can accustom ourselves to observe our BG patterns with varying levels of movement, intensity, and duration and adjust our treatment strategies accordingly. These methods can help us focus less on diabetes and more on what really matters…channeling our inner strength for those PR’s!


I’m reading ur article .
I am having such a hard time exercising .. i have been working with my diabetes educator and nutritionist and we can’t get a consistent balance. I wake up the same time every day eat the same foods , exercise pretty much the same way and every day it’s a diff story.
I run for around 1 hour..a lot of hills, somedays I feel good and most days my sugar goes high . My runs have become frustrating . When it’s high I can’t get oxygen to my leg muscles and I can’t run I have to stop ..
I get this high sugar spike ( which is when I feel the exhaustion, then a steep decline. )
Can anyone help me ?
Hi Rachael, check out this article from Gary Scheiner who lives with type 1, is an exercise enthusiast and also has a company dedicated to helping people living with diabetes:
https://diatribe.org/sports-and-exercise-ultimate-challenge-blood-sugar-control
Hi Rachael. Thank you for reading my article! I’m sorry you’ve been having trouble trying to maintain your blood sugars during exercise. For me, I stick with the same trail and distance, alternate between running and walking, keep about the same pace, and I find that with little or no insulin on board, my blood sugar is usually stable. And yes, I agree with TCOYD- Gary Scheiner is fantastic- be sure to check out some of his articles. He also had a great book called “Think like a pancreas.”