
- The push toward a functional cure for T1D continues to gain momentum. Vertex’s Phase 3 trial using stem cell-derived islet cells is already underway, and Kriya Therapeutics’ AAV gene therapy trial is gearing up to start later this year.
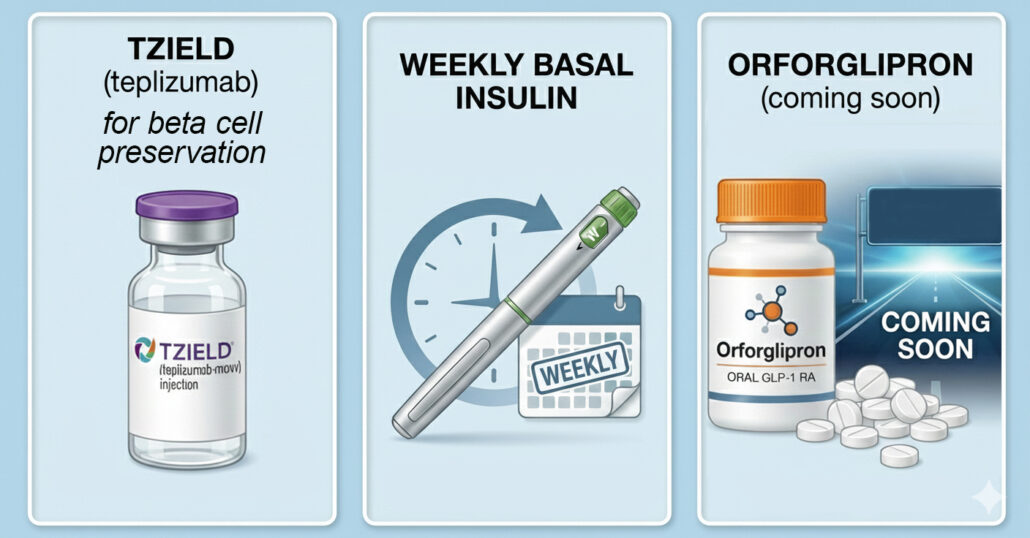
- Tzield will likely be approved as a treatment for those newly diagnosed with type 1 diabetes, making it the first FDA-approved medication to preserve beta cell function in newly diagnosed T1D. It’s already approved to treat people in Stage 2 T1D.
- Diabetes medications will continue to evolve, from new dual and triple agonists for type 2 diabetes to the possible approval of inhaled insulin Afrezza for kids with type 1 diabetes.
- Advances in type 2 diabetes treatments like once-weekly basal insulin may become a viable option, offering a simpler alternative that reduces the burden of daily injections.
- In diabetes technology, we expect FDA approval of the first continuous ketone monitoring system, a new (and smaller) insulin pump from Medtronic, smarter AID algorithms, and expanded pump and sensor integrations.
Reading Time: 4 minutes
The Magic 8 Ball in our production studio is pretty accurate when we ask it crucial questions like, “Should I have another handful of M&M’S even though I’m already a little high?” It always faithfully responds, “All signs point to yes.”
For this article, though, we went straight to our human inside sources (Dr. E and Dr. P) to find out what we can really expect to see in 2026.
New Diabetes Drugs and New Medication Indications
First Therapy to Preserve Beta Cell Function in Newly Diagnosed Type 1
Any day now, we’re expecting Tzield to be approved by the FDA to preserve beta cell function in people newly diagnosed with type 1 diabetes (Stage 3 T1D). Tzield has already shown prevention (it’s approved to treat people in Stage 2 T1D) and the next step is preservation. Most people still have about 10-20% of their insulin-producing beta cells at diagnosis, and research shows Tzield can protect those remaining cells. If approved, it would be the first therapy to preserve beta cell function in those newly diagnosed.
An Easy Pill to Swallow: New Oral GLP-1 for T2D
Orforglipron is a promising new oral GLP-1 developed by Lilly for type 2 diabetes. It’s a once-daily pill that acts similarly to an injectable GLP-1 like Mounjaro. Studies show impressive results in both glucose control and weight management. Since it can be taken without food and water restrictions, it could make life a lot easier for people who want the benefits of a GLP-1 without injections. We expect it to be approved by the FDA in 2026.
Next-Level Ozempic for Type 2 Diabetes: CagriSema
CagriSema is Novo Nordisk’s newest heavyweight drug for type 2 diabetes. This once-weekly injectable combines semaglutide (the same ingredient in Ozempic and Wegovy) with cagrilintide, creating a next-level GLP-1 therapy.
Semaglutide mimics the GLP-1 hormone to lower blood sugar, reduce appetite, and promote weight loss. Cagrilintide adds another powerful layer by mimicking amylin, a natural hormone that further helps to reduce post-meal glucose values, reduce appetite, induce satiety, and lead to weight loss. It’s given weekly in a similar manner as Symlin (generic name pramlintide) which is injected 1-3 times per day, so it’s a much better form factor. CagriSema is working toward FDA approval in 2026.
A Triple Threat for T2D and Obesity: Retatrutide
Retatrutide (nickname “Triple G”) is a new medication from Lilly that mimics three hormones – GLP-1 RA, GIP, and glucagon – which is more than any GLP-1 medication to date. Stimulating glucagon helps to prevent muscle loss, which is important when you’re taking a GLP-1 medication. Data released from Lilly’s TRIUMPH-4 study on December 11th showed that retatrutide lowered weight by up to an average of 28.7% (71.2 lbs) at 68 weeks (with an average baseline weight of 248.5 lbs), and study participants also had substantial relief from osteoarthritis pain. Retatrutide is being studied to treat type 2 diabetes, obesity, knee osteoarthritis, and sleep apnea, with a simultaneous FDA submission hopefully this year.
Weekly Insulin for Type 2 Diabetes
Once-weekly basal insulin for type 2 diabetes is inching toward reality, and we think 2026 will be the year it gets approved. The data looks good for both Lilly’s efsitora alpha and Novo Nordisk’s insulin icodec. In recent studies, they performed just as well as today’s best daily basal insulins, with no extra hypos. Weekly basals did cause more hypoglycemia in T1D trials, so it probably won’t become an option in type 1 anytime soon.
GLP-1s Expand Their Side Hustles: Heart, Kidney, Liver…What’s Next?
The fab four of GLP-1 RAs – Ozempic, Mounjaro, Wegovy, and Zepbound – started out as treatments for type 2 diabetes and weight loss, respectively, but they quickly added other treatment areas to their resumes. Even more indications are expected, and will likely include treating prediabetes, knee osteoarthritis, Alzheimer’s disease, and drug addiction.
GLP-1s for Type 1s Are So Close We Can Taste It!
Studies are ongoing testing GLP-1 medications in type 1 diabetes…finally! Lilly is holding trials with Mounjaro, and Genentech is studying their dual GLP-1/GIP agonist CT-868. Many HCPs already prescribe these medications off-label for people with type 1, and patients are seeing significant weight loss, better blood sugars, and reduced insulin requirements.
The first FDA approval may not come until 2027, but we hope it will set off a domino effect that brings more medication options for T1D down the pipeline.
Medicare Offers $50 Copay for GLP-1s
People on Medicare with severe obesity will soon be able to access Zepbound or Wegovy (the weight loss versions of Mounjaro and Ozempic), for a $50 monthly co-pay. The new pricing could take effect as soon as April. Medicaid pricing and timing will be dependent by state as they opt in.
Updated Dosing Guidelines for Inhaled Insulin Afrezza
Afrezza has been around for about a decade, but it’s finally getting the credit it deserves. It gets into your system fast and wears off fast, so it’s very helpful for reducing post-meal blood sugar spikes and minimizing delayed lows.
When Afrezza first launched, the dosing was one-to-one with rapid-acting insulin, but that turned out to be too conservative. New dosing recommendations are now on track for FDA approval this year.
Needle-Free Insulin for Kids Ages 4-17
MannKind’s application for inhaled insulin Afrezza for use in kids was submitted to the FDA in October, backed by strong Phase 3 INHALE-1 results showing it’s safe and works well for children ages 4 to 17. If the FDA gives the green light, kids (and parents) could soon have a needle-free insulin option.
New Diabetes Technology

(Pictured above: Medtronic’s MiniMed Flex and MiniMed Fit insulin pumps)
The biggest tech news of the year will likely be the approval of Abbott’s continuous ketone monitoring system, but keep an eye out for new pump options from Medtronic, multiple AID algorithm advancements, and additional pump/sensor integrations.
A New Way to Prevent DKA: Continuous Ketone Monitoring
Abbott’s new combined continuous ketone monitor (CKM) and CGM is going to be a big deal because it will notify you of elevated ketones before an emergency situation like diabetic ketoacidosis (DKA) occurs. The ketone monitor function will also allow people with type 1 diabetes to take an SGLT inhibitor (like Jardiance, Farxiga, or Zynquista) safely, which could pave the way for FDA approval of these medications in T1D.
Two New Pumps from Medtronic
Medtronic is expanding its AID lineup with two new insulin pumps. MiniMed Flex, a small, screenless tubed pump, has already been submitted to the FDA, and MiniMed Fit, a tubeless patch pump, will likely be submitted in late summer/early fall. Both systems will run on a new algorithm called Vivera, and pair with the Simplera Sync and Instinct sensors.
Cure-Based Approaches for Type 1 Diabetes

2026 may not see a “cure” for type 1 diabetes, but we anticipate positive data from Vertex’s Phase 3 stem cell-derived islet cell therapy study, and Kriya’s first human gene therapy trial, which is expected to start later this year.
Stem Cell-Derived Islet Cell Transplantation
Vertex’s VX-880 (also called zimislecel) is a groundbreaking treatment for people with type 1 diabetes that aims to help the body make its own insulin again. It uses lab-grown islet cells placed in the liver, where they work like real pancreatic beta cells.
People currently need immunosuppressive drugs to protect the new cells, but researchers are working on ways to avoid those medicines in the future. VX-880 is now being tested in large Phase 3 studies, and we expect the company will submit applications to regulators later this year.
Human Trials for T1D Gene Therapy
Kriya Therapeutics will begin human trials this year for their investigational T1D therapy KRIYA-839. It works by using a benign virus to deliver genes for human insulin and a glucose-sensing enzyme called glucokinase into muscle cells, essentially teaching those muscles to help regulate blood sugar the way healthy pancreatic cells do. In animal studies, this approach normalized blood sugar levels and lowered A1C, without causing lows and without immunosuppressants.
Key Takeaways: New Diabetes Drugs, New Diabetes Technology, & Progress
2026 will definitely be a year of progress, with advances in type 2 diabetes treatments, continuous ketone monitoring that may lead to approvals of SGLT2s for type 1s, expanded insulin pump choices, smarter AID algorithms, and continued momentum toward a cure for type 1 diabetes. The future is clearly moving in the right direction…forward! 😉
Explore our resource library and video vault, and subscribe to our monthly digital newsletter for tips, tools, and expert guidance on how to take control of your diabetes.

Our goal is to protect your personal health information. Please keep your questions general and do not post personal medical information here. If you have a specific question, please email events@tcoyd.org.