Good news! The diabetes world no longer revolves around the A1c. Time-in-range and glucose variability play a much greater role. We also know more than ever about the harmful effects of after-meal blood sugar spikes.
What’s a Blood Sugar Spike? And Why Do They Happen?
Postprandial spikes are temporary high blood sugars that occur soon after eating. It is normal for the blood sugar to rise a small amount after eating, even in people who do not have diabetes. However, if the spike is too high, it can affect your quality of life today and contribute to serious health problems down the road.
The reason blood sugar “spikes” is a simple matter of timing. In a non-diabetic, consumption of carbohydrate results in two important reactions: the immediate release of insulin into the bloodstream, and production of a hormone called amylin which keeps food from reaching the intestines too quickly. In most cases, the after-meal blood sugar rise is barely noticeable.
However, in people with diabetes, the situation is like a baseball player with very slow reflexes batting against a pitcher who throws 98 mph fastballs: the timing is not good. Rapid-acting insulin that is injected (or infused by a pump) at mealtimes takes approximately 15 minutes to start working, 60-90 minutes to “peak,” and four hours or more to finish working. And don’t forget about the amylin hormone effect. In people with diabetes, amylin is either produced in insufficient amounts or not at all. As a result, food digests even faster than usual. The combination of slower insulin and faster food can cause blood sugar to rise absurdly high soon after eating. This is followed by a sharp drop once the mealtime insulin finally kicks in.
Why Are Blood Sugar Spikes a Problem?
Even though the spike is temporary, all of those spikes throughout the day can raise your HbA1c. Research has shown that for those with an A1c below 7.5%, post-meal readings actually have a greater influence on A1c than fasting blood sugars. In other words, managing pre-meal readings will only get you so far. If you want tight control, you need to pay attention to the after-meal glucose as well.
The long-term effects of postprandial hyperglycemia have been studied extensively. For those with type 1 diabetes, significant post-meal rises have been shown to produce earlier onset of kidney disease and accelerate the progression of existing eye problems (retinopathy). And like a dagger through the heart, post-meal hyperglycemia is an independent risk factor for cardiovascular problems. Recently, post-meal spikes and glucose variability have been associated with diminished brain function and an increased risk of dementia.
But the problems are not limited to long-term health issues. Any time blood sugars rise particularly high, even temporarily, our quality of life suffers. Energy decreases, cognitive (thinking) ability falters, physical/athletic abilities become diminished, and moods become altered. And don’t forget: What goes up must come down. The rapid blood sugar decline that usually follows a post-meal spike can cause false hypoglycemic symptoms.
Blood Sugar Measurement & Goals
The exact timing of blood sugar spikes can vary from person to person and meal to meal. However, on average, the post-meal peaks tend to be about one hour and 15 minutes after starting a meal. But the best way to measure post-meal patterns is by using a continuous glucose monitor (CGM). These systems, available from Medtronic, Dexcom, Abbott and Senseonics, provide glucose readings every couple of minutes so you won’t miss the peak, whenever it happens to occur.
So exactly how high is TOO High? There is no universal answer. The American Diabetes Association recommends keeping blood sugar below 180 mg/dl 1-2 hours after eating. However, no specific guidelines are provided for type-1 vs. type-2 diabetes, insulin users vs. non-insulin users, or children vs. adults.
Based on my experience, I usually recommend the following:
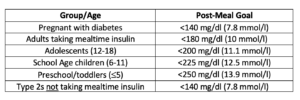
Post-meal readings that are consistently above these levels should be addressed by you and your healthcare team (see strategies in the sections below).
How to Control a Blood Sugar Spike
To reduce the spike, a number of strategies can be used. Some involve medications while others involve our lifestyle choices. Here are a few medical approaches:
1. Choose the Right Insulin
The right insulin can make or break your ability to control those after-meal spikes. In general, insulin that works quickly and for a short period of time will work better than those that work slowly over a long period of time.
For instance, rapid-acting insulin analogs (Humalog, Novolog or Apidra) will cover the post-meal blood sugar rise much better than regular insulin. Newer ultra-rapid insulins, such as Fiasp, work even faster.
The way insulin is administered can dramatically affect its speed of action. Afrezza is an inhaled insulin that can be used at mealtimes. Because the dry powder is absorbed through the lungs, its onset and peak are much earlier than injected insulin. For those who don’t mind a twinge of pain, injecting insulin into muscle will also make it absorb and act much quicker than injecting it into the fat layer below the skin.
Research has also shown that injected insulin can work much faster when the injection site is warmed by rubbing the site, immersing in warm water, or exercising the muscle near the site. Warming the site causes the blood vessels near the skin to dilate, which allows the insulin to absorb more quickly. By the way, smoking causes the blood vessels to constrict, so quitting smoking might improve your post-meal blood sugar (in addition to helping you and those around you to live longer).
2. Back Up Your Bolus
For those taking rapid-acting insulin at mealtimes, the timing of the injection (also called a “bolus”) can have a huge impact on the after-meal spikes. Unless you suffer from gastroparesis, it is best to give boluses before eating. How long before? It depends. The higher your blood sugar, the earlier the bolus should be given. With a pre-meal blood sugar that is well above-target, it is best to give the bolus and then wait 30 minutes before eating. Near your target blood sugar? Wait 15 minutes. Below target? Take the bolus and eat right away. Research has shown that simply giving mealtime boluses before eating rather than after can reduce the post-meal spike by an average of 45 mg/dl.
3. Bolus for the Basal
In order to have more insulin working right after eating and less working several hours later, a pump user can run a substantial temporary basal reduction for 3 hours just before eating and give a normal bolus equal to the basal insulin that would have been delivered. John Walsh, coauthor of the Pumping Insulin books, calls this a “Super Bolus”. For example, if your basal rate in the morning is .6 units per hour, you could bolus an extra 1.8 units before breakfast and then set a temp basal of 10% (90% reduction), for the next 3 hours.
4. Choose the Right Medication
Two classes of injectable hormones, GLP-1 receptor agonists and amylin mimetics, have powerful effects on post-meal blood sugar. Both GLP-1s and Symlin slow gastric emptying and keep carbohydrates from raising the blood sugar too quickly after meals. Symlin, which is a replacement for the amylin hormone (which is lacking in people with diabetes), also helps to diminish appetite and blunt post-meal glucagon secretion. GLP-1s blunts appetite and promote the growth of insulin-producing cells in the pancreas of those with type-2. So both can contribute to better post-meal blood sugar control.
For type-2s, the choice of oral medication can also impact your after-meal control. Sulfonylureas stimulate the pancreas to secrete extra insulin throughout the day, without regard to meal timing. There are alternative medications called meglitinides which also stimulate the pancreas but do so in a much faster and shorter manner. When taken at mealtimes, meglitinides produce better after-meal control than sulfonylureas.
Lifestyle Approaches to Stop Blood Sugar Spikes
1. Think Lower GI
Glycemic Index (GI) refers to the speed with which food raises the blood sugar level. While all carbohydrates (except for fiber) convert into blood sugar eventually, some do so much faster than others.
Many starchy foods (breads, cereals, potatoes, rice) have a high GI; they digest easily and convert into blood sugar quickly. Some starchy foods (pasta, beans, peas) have lower GI values. Foods that have dextrose in them tend to have a very high GI. Table sugar (sucrose) and fructose (fruit sugar) have moderate GI values, while lactose (milk sugar) is slower to raise blood sugar. A number of books, such as Dr. Jennie Brand-Miller’s Glucose Revolution series, contain extensive information about the glycemic index, along with lists of GI values for hundreds of foods.
As a general rule, switching to lower-GI foods will help to reduce your after-meal blood sugar spikes.
Below are some examples of ways to substitute typical high-GI foods for lower-GI options:
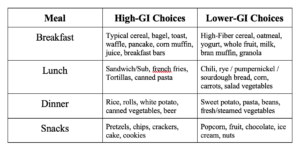
Another unique food property that affects rate of digestion is acidity. This is why sourdough bread has a much lower GI value than regular bread. Research has shown that adding acidity in the form of vinegar (straight or in dressing/condiment form) can reduce the one-hour post-meal blood sugar rise by 50% or more.
2. Split Your Meal
When having a full meal or large snack, consider saving a portion for one or two hours later. Still give the full mealtime insulin before eating any of the meal; just don’t eat all of the food at once. For example, if you have a bowl of cereal and juice for breakfast, considering having the cereal at breakfast time, and postpone the juice until mid-morning.
3. Get Moving
Physical activity after eating can reduce post-meal spikes by diverting blood flow away from the intestines, resulting in slower absorption of sugars into the bloodstream. Plus, the sugar that does enter the bloodstream is likely to be “consumed” by the working muscles. It doesn’t take much activity: Ten or 15 minutes (or more) of mild activity will usually get the job done. The key is to avoid sitting for extended periods of time after eating.
4. Prevent Hypoglycemia
Low blood sugar is problematic in many ways. One of the body’s typical responses to hypoglycemia is accelerated gastric emptying: food digests and raises blood sugar even more rapidly than usual. Prevention of hypoglycemia prior to meals and snacks is yet another effective strategy for controlling post-meal blood sugars.
Gary Scheiner MS, CDE is Owner and Clinical Director of Integrated Diabetes Services, a private practice specializing in intensive insulin therapy. He is author of several books, including Think Like A Pancreas: A Practical Guide to Managing Diabetes With Insulin, and was named 2014 Diabetes Educator of the Year by the American Association of Diabetes Educators. Gary has had Type-1 diabetes for 34 years. He and his team of Certified Diabetes Educators consult with people throughout the world via phone and the internet. He can be reached at gary@integrateddiabetes.com, or +1 610-642-6055.
Additional Resources
Post-Meal High Blood Sugars: How to “Strike the Spike”!
Inhaled Insulin Afrezza: An Underutilized Treatment in the Type 2 Toolbox
How to Pump for Pizza (and other high-fat foods)


Dear Dr. Schneider, thanks as always for all this great advice. The combination of getting onto a Dexcom GCM and working with your team a couple of years ago has brought my A1c down to 6.8 (Down by 0.8 points) and my time-in-range is 87%. When I am anxious (for example, a few days before traveling), my BG keeps spiking, so I read this article with great interest. Perhaps you can address stress and ramifications (as well as ways to cope with the resulting high BG) in a future article. Thanks again!!
Thank you for your comment, Carol, and great idea for another article.
Super helpful! Knowledge is power. Thanks! I am a type 1- actually I have LADA. Spikes are terrible problem for me . Hopefully, this info will help.
We hope so too Judy! 🙂
Thank you so much for this information. It is easy to understand and helps me to work on something I have been noticing and wanting to improve.
Thank you Valerie – hope it helps. 🙂
I have been doing the protocol of the exercise (walking) within 1-1.5 hours after the first bite of food, decreasing high glucose dumping foods, for the last 8 years with my patient’s and getting A1C’s <7 in type II diabetics, often without meds (except Metformin at least) and no hypoglycemic. Favorite DM meds are the incretins. So glad to know that others are doing this too. I tell my patient's that we want to stop the wrong foods coming in the mouth to start with, so that we can decrease their costs and control the disease. It really is working and it is so exciting to see the empowerment of the patient.
This is a great article. So many great tips presented with the science behind them.
Very interesting and helpful since I have problems with post meal spikes. I am type 1 on a pump and cgm.
When do you take the vinegar and how much?
Thanks.
Hi Gail, according to Gary Scheiner, 1 tbsp vinegar a few minutes before a meal should do the trick.
Do you have any guidelines you would suggest for a BG range for a teen driver with Type 1? For example BG should be between 100-200 or something similar?
Not sure if this is an official recommendation but I think having a CGM with a lower alert alarm set at 80mg/dl is the safest way to go. A BG between 140 and 180 is also very safe, but once again you could be 150 and dropping quickly and with out a CGM that could be dangerous.
Very helpful. I had not heard of the Amylin effect for T1D. Makes sense. I thought the stomach has the fastest absorption of sugars, over the intestines. I like the food comparison charts. I do oatmeal, with concern, but only looked at carbs. The body is complicated and an amazing design. Dexcom G6/is helping to better understand the changes, finally for aT1D of 34 years.
Hello Dr. Gary
I was diagnosed with gestational diabetes and after birth, blood glucose will rise 180s and drop 50s after 4 hours. My endocrinologist said it’s type 1 diabetes after running some labs. I am not take any medication, but constantly dropping and I have to keep eating even in the middle of night; I gain weight from eating too much to keep the glucose up. Thyroid function normal. When I exercise, the glucose drop faster. Recently took diazoxide, but didn’t help. Please I need your point of view. Thank Dr.
This situation is unusual and it’s hard for me to comment. Make sure you are seeing an endocrinologist who knows about excess insulin production.
Hi,
Thanks for your article and all the comments. I have a question. I am 85, slim, active but I have problems with BG spikes. My A1c level is well within acceptable range, 37 mmol/mol. I control the BG by avoiding sugar and white carbs. Is this kind of thing normal for oldies?
regards
Dan Pallant
Totally normal, Dan. Keep up the good work!
Is it normal for your blood sugar to be in the upper 140 range 3 to 4 hours after
Consuming 60 to 80 grams of complex carbs
It could definitely be in the realm of normal, especially if you’re eating those carbs with protein and fat.
For a diabetic not on insulin, what is the goal 1-2 hour after meals?
Hi Stanley, Gary mentions this in the “Measurements & Goals” section of the article, and adds his recommendation in the chart provided.
Thank you.
Hi im joey im in nc my mom is typ 2 she is 72 she btms out then spikes in evening.around 340 it scares me tried change diet 3 meals day healthy food dont help lots water l need help my email rashtrans01@gmail.com
Joey…if she bottoms out consistently for sure she needs an adjustment in her insulin dose. Make sure her doctor knows this information.
Great article! I’ve found the most effective way of keeping my blood sugars steady is drastically lowering my refined carbohydrate intake and following a high protein, low carb lifestyle. My A1c has reduced to 5.4% (the same as a non-diabetic) and for the last 3 weeks I have had no hypos whatsoever. I haven’t spiked above 8 mmol / 144 mg/dl for the past 90 days. Completely life changing!
Wow, Sophie, congrats to you!
Dear Sophie
Are you on meds still and how long have you been diabetic?
Hi Karl, I’ve had type 1 diabetes since 2013. I still have to take insulin injections daily, but I now take 50% less bolus and basal insulin than I did when I was eating higher carb. I follow something called ‘The Law of Small Numbers’: small amounts of carbohydrates – require small amounts of insulin – which means small chances of error.
Recently, my Endocrinologists, at UW medicine, both Attendee and MD fired me as a patient in the middle of treatment(I am on meds). I suppose it is because they simply hated that I have some knowledge and they cannot answer to my questions. I have huge spikes whenever I eat cabs, like 250s at one hour. it will go down to 140-150 at two hour(no, its not perfect). I had hypoglycemia 1 year ago(like 45), but not anymore(which means less insulin now). My fasting was 70-80 one year ago, now hitting 100s at times, and maily 90s. When I eat blueberries(low GI, 34), it was only 100-120 one year ago, now it is hitting 160 at one hour. my BG is obviously getting worse. While I sleep, BG going up somehow around 3AM. My A1c is 5.1%, I know I am very healthy at this point, im thin woman at her 30s, always fit in my life. Im from Japan, In Japan, there are many diabetes who are thin, and fit, so I explained them, but they never listened me. There are some researches that if you start meds at pre- stage, it may “cure” ( really) the spike so I begged them, and now I am now on Januvia but not really seeing a result, anyway they fired me so what to do….. Wishing to be pregnant, but if ill be now, of course high risk of Gestational diabetes, so really concerning now. Those doctors told me “its just stress, eat carbs, stop checking BS, bring up your a1c to 5.8% then we can think from there, over 200 at one hour is normal for thin women like you”. I was jaw dropping. I do exercise a lot, burn 200kcal daily on treadmill plus muscle training, and eat healthy with lots veggies. but my BS keep getting worse and I do not know WHY. any idea? If it is stress, HOW TO STOP IT??? thats my question and they could not answer but fired me. I know it is not emergency situation, but I dont wanna be diabetic.
It sounds like you need a sympathetic, nice diabetes doctor. Your goal should be less than 7%, so do not stress at 5.8% You really need to watch some of the videos on type 2 diabetes in our video vault:
https://tcoyd.org/video-vault/
Watch the one I did called “There has never been a better time to have type 2 diabetes.” It is normal for blood sugars to go up over time…it is called the natural progression of type 2 diabetes.
Thank you Doctor for your time.
So personally, you think that I should keep seeing a diabetes doctor, correct? That’s what exactly I think, and the ADA person I spoke also told me that I should keep following up with doctors if I am hitting over 200(or even over 160) when I eat carbs. Of course, I’m not planning to see a doctor every month, but as my fasting and all the BS getting worse, I believe that I should keep monitoring it with a specialist, and not trusting those UW medicine MDs who told me I should not come back anymore to specialists.
Yes, it’s important to find a healthcare provider you trust and feel comfortable with.
Thank you, that’s what I thought…. Can’t believe how come those doctors told a patient who is hitting over 250 “no need to come back to see a specialist”…. It is really important to have the real doctor who is really knowledgeable about their specialities.
Dear Dr. Schneider, thank you very much for the useful information. I am 59 year old (female), diagnosed with type 2 diabetes 3 months ago with a1c 6.3, fasting blood sugar 5.1 and the oral glucose tolerance test 15.5. Since then I have taken low carb diet, doing more exercise and reduced weight 5 kg in 3 month and get my a1c to 5.5 this week.
Today I had lunch with some noodles. Before lunch the blood sugar was 4.2. Two hours later after lunch, it’s 14.5. Three months ago, the blood sugar was 14.8 after taking the same noodles. It looks like I have normal fasting blood sugar and a1c, but can not take sugar challenge. Can you advise what I should do to improve? Many thanks.
Hi Meiyun,
Gary runs an organization called the Integrated Diabetes Services and it sounds like you might benefit from working with him and his team. You can reach out Gary and his staff here:
https://integrateddiabetes.com
https://integrateddiabetes.com/contact-form/
PHONE: (610) 642-6055
TOLL FREE: (USA) 877-735-3648
Outside the US: 001-610-642-6055
Good luck!
I am 22 years old and I was gestational diabetic and after delivery now my fasting sugar is below than 100 and after 2 hours of breakfast intake my sugar range is less than 140 am i still diabetic please guide me
According to the guidelines, your values are normal.
Hallo, is it normal for my blood sugar to spike to 9-11 just after my food with some meals. It is about 7.8 an hour or 2 after meals again and then less than 6 after 2 hours. Sometimes I dont feel well minutes after eating then my sugar is high but is it not normal if you had a very sugary meal that it would be very high? Im not diagnosed with diabetes but I do have some concerns. The doc told me 5 years ago that I need to check my sugar regularly because my baby weighed 4.05kg at birth and that is a sign I could be pre diabetic.
Some of those numbers are fairly normal for someone without diabetes, but the higher numbers are abnormal. Typically people without diabetes do not get above 10 mmols/L (180 mg/dL) after eating. You may have prediabetes. It would be good to check your A1C.
I had fasting sugar 94 I ate 2 ripe mangoes and after 2 hours I checked, it was 127.afternoon meal I had 4 bajra roti and Parwal vegetable and mix dal, after 2 hours my sugar lvl was 216. Why this happened
Your numbers did not rise too high after eating fruit, but 216 is above the goal for people with diabetes (though still not too high). If you have diabetes, it’s good that you are paying attention to which foods cause a high rise in blood sugar.
I am 72 years old, female. Four years ago, after reading “The Obesity Code” I started my journey towards a normal BMI. My BMI was 28, over weight. I started with a low carb diet, then to Keto, and now intermittent 8/16 fasting. I did not exercise regularly. I lost 10 lbs. However, My A1C went up from 5.7 to 6.2 within 1 year. I assumed eating low carb and fasting would keep my A1C under 6. I assumed I could have cheat days on holidays and birthdays. I wanted to figure out why my A1C went up, so I started to eat to my meter. Ice cream, cake, corn dog spikes my blood to 190. Apple spikes my blood to 160. Testing 2-3 hours after first bite, when I return home. My fasting BS is 120’s . ( I have dawn effect) After 40 minutes of exercise, still fasting my BS is 130’s.
After a 24 hour fast, my fasting BS is still in 130’s. After I eat at noon, my BS drops to 110 – 120. My bedtime BS is around 110.
My question: Can a person be healthy and still have occasional spikes around 190’s if my bedtime BS is normal?
Absolutely yes!
Very informative and useful article ,practices tips on management of diabetes
Hi,
Do non-diabetics get these meal spikes?
I’ve not been diagnosed and yet to talk to my doctor but looking for some informed advice.
I had cereal this morning (Coco Pops ) with milk mixed with a scoop of Protein powder and around 30 minutes later my BG went up from around 5.2 to 9.1
I have a CGM and so with the alarm going off, I went for a 10 minute walk around the block. It came down to 7.2. 10 minutes later it was down again to around 6.3 however, another 10 minutes later was up to 7.3.
Trying to understand what ‘safe’ levels are, maybe if I’m pre-diabetic even.
You are in a safe zone, but you may have pre-diabetes.
Hi,
I have been diagnosed with diabetes like 10 months ago. I was on insulin and metformin. But still doc couldn’t find out whether I am T1 or T2 because T1 antibodies are negative and my pancrease doesn’t produce too insulin which is currently under the range(c-peptide). Currently doc changed my medication to januvia, metformin 1000mg and optisulin 8 unit, but doc asked me to stop using long acting insulin. I tried to stop it but my fasting sugar (7-8 mmol) and after meal time sugar goes high (9-11). Day time is ok but after dinner it always goes high it doesn’t matter how much food or low GI food I eat. Could you suggest what actually could be the problem?
It is really hard to say what may be going on without a lot more information/tests. I would see a good endocrinologist who specializes in diabetes. Your diagnosis could range from insulinopenic type 2 to antibody negative type 1, but just cannot say based on the information you gave me. Good luck.
Dr Edelman
Thank you for the opportunity to ask questions. I have been type 2 diabetes for years now: I had been on synjardy but dr switched to 25mg jardiace because of diarrhea, During the day I can control my blood sugar levels even without med. However my morning fast is always very high 160-210. This happens no matter what I do before going to bed. I am very concerned about this. Any suggestions how to get lower fasting levels. Thanks so much
There’s lots of other choices out there. You can do the long-acting metformin, which causes less diarrhea, but also a GLP-1 RA would also be a good addition. There are more choices than that…email lynne@tcoyd.org and she can send you a digital copy of my TCOYD book.
Good afternoon! Thank you for all of the information you have provided on your website, it is GREATLY appreciated. I do have a few questions and I will try to keep it short. First of all a bit of back history..my sister, my mother, her parents and siblings, her grandparents and so on all have T2D. I am 5’2″ and am now only 105lbs, 6 months ago I was around 115lbs. I am a very healthy eater, so what I eat is not an issue. I have always been hypoglycemic with lows sometimes in the 40’s.
Just over the last 6 months I have noticed I have been getting seriously exhausted. Even walking my little dog around the block wears me out so much I feel like I am going to pass out. I have always checked my blood sugar and know the feelings of hypo’s, this feeling is very different! I talked to my doctor and asked her for a CGM. She gladly gave me one 2 months ago and had me get my A1c checked. It was at 4.9. 2 years ago when I had my A1c checked it was below 4.0, I don’t remember the exact number. I started checking my BS and noticed that I have had a lot more highs (160’s+) than the lows I am used to experiencing. My doctor looked at all of my numbers from my glucometer and CGM and suggested I go see an endo, she believed I may be converting to type 1.5. When I went to see the endo, she just told me I am not diabetic and it is impossible that I have ever been hypo. She just kept telling me what she sees is normal. After me continuing to try to get her to listen, she reluctantly sent me over for a glucose tolerance test. Well, come to find out, my 2 hour showed my BS was at 220 and she said I was pre-diabetic and put me on Metformin ER 500mg for the first week and 1000mg starting next week.
So, here are my questions…
1) I know it is possible for a hypo to develop diabetes, however, during the “conversion time” would the A1c show to be normal? The way I picture it is if a person has BS say at 40 for 1.5 months straight then say at 280 for 1.5 months, the A1c would show normal – right?
2) I just started Metformin just a few days ago on 10/2/21. I have been getting even more exhausted and feeling like I am either high or low BS, yet when I check my BS shows mostly between 80 and 90. Does Metformin keep BS stable? What is going on with these high and/or low feelings? Are these weird feelings normal side effects of Metformin? All I have been able to find is the stomach issues.
3) Not necessarily a question, but I have a feeling this is the start of LADA vs T2D. I will be going through your website to learn more about this. Any helpful tips you can give to help me through figuring all of this out?
I thank you for your time and again, I appreciate what you’ve done on your website.
Hi Diana,
Thank you for reaching out. To answer your questions…
1) That is definitely possible. The glucose levels are all part of a continuum, so it’s definitely possible.
2) Those high and low feelings are definitely not a side effect of Metformin. Metformin has been around for 50 years. Your high and low feelings are real, but they may just be temporary.
3) With your family history, I would bet that it’s early type 2 diabetes, because it runs very strongly in family members. But the most important thing at this point is to keep an eye on your blood sugars and follow them so they don’t get excessively high. And if you are responding to Metformin, then it means you have type 2. With LADA/type 1 you will ultimately need insulin.
Dr Elderman
I have only just come across your website, and it makes a lot of interesting reading.
My wife has been type 2 diabetic for a good number of years, however last june (2020) she managed
to get prediabetic readings.
Obviously my wife was overjoyed.
However a blood test in September (2021) showed mmol/mol of 101.
The doctors were extremely concerned, but have no idea how this.
My wife has not changed her diet for a number of years, and keeps away from anything with sugar, and cutting down on carbs.
I recently bought a monitor, to keep a continuous test regime, and and for some unknown reason
her readings for mmol/mol has dropped to 51. Whic hopefully is good news.
However, I have noticed a pattern that no matter what my wife eats for breakfast, there is always a spike which is way above the norm. There are no spikes any other time of the day. The spike lasts for approx. 2hrs.
My wife takes gliclozide in the morning with a metformin tablet, then 2 metformin tablets in the evening.
This is causing some concern for my wife, and would appreciate, any advice as to the way forward please.
Thank you
Frank
Hi Frank,
She can try eating a breakfast with extremely low carbs, and/or try to spread the calories out over the course of the morning if she can and if it’s practical, so she’s not introducing all the food at once. Depending on how high she goes, she may not need to do anything if her A1c is good.
Diana
Thank you for the prompt response.
Thankfully at present with controlling what my wife eats, her glucose levels
are being maintained in the green area for 80% of the time, it is only the morning
spike lets the overall readings down.
We will persevere but the godsend is the CGM, which certainly helps monitoring
and subsequently controlling of the diabetes.
Thank you again, and hopefully your site is helping
a lot of people with their concerns over diabetes.
Wow, great reading even for a non-diabetic! I have idiopathic neuropathy and trying to eliminate some of the possible causes for this nerve damage. Blood sugar issues are clearly a concern and many diabetics develop neuropathy. I received info from a Functional Medicine MD explaining the damage that blood sugar spikes can cause. Apparently, spikes (and crashes) stress the adrenal glands aggravating the autoimmune system and creating inflammation in the body that can ultimately damage tissues. For that reason, this MD uses a Continuous Glucose Monitoring System on all patients.
My PCP and Neurologist seem satisfied to leave my diagnosis as “idiopathic”, but I prefer to seek out the possible causes, mainly by eliminating the issues that are NOT creating problems. I have a family history of late onset diabetes and had gestational diabetes when pregnant, so figured this was an issue to look at. But, with basic blood work showing normal A1C now, I had to really convince my doctors to look further. The best I could do was a 2 hr. glucose tolerance test. But, I think that was enough, wondering if you might agree.
I am a 71 year old female. My A1C tests at 5.6. Fasting glucose tested at 91, spiked to 106 at 1 hour and back down to 91 after two hours. After reading this article, I’d say those test results are a good indication that the concept of blood sugar related issues is not likely causing the neuropathy. Apparently my body handles glucose properly. Would you agree or am I over simplifying the situation???
I’m sure my doctors would love to say I told you so, but it seems to me that a normal A1C is not necessarily the final test of blood sugar related issues. I believe the information in this article is pertinent to non diabetes as well as diabetics and really appreciate the education I received! Now on to other possibilities aren’t being addressed as well as I’d like; a mild car accident, hip surgery, and possibly, even, that partial colon removal I had as a child! As long as I don’t obsess over these things, I see no harm in curiously seeking out the cause of this condition. And look what I’m learning along the way!
Thank you for your insight!
Your glucose numbers are absolutely normal and not the cause of your neuropathy. There are more causes of neuropathy than any condition that we know of. Sometimes if we don’t have a solid reason, we call it idiopathic. It’s extremely common with neuropathy that we just don’t know what the cause is. Everything from toxins to smoking to chemotherapy to uncontrolled diabetes…and many more conditions. I suggest putting into google “differential diagnosis of peripheral neuropathy” and you will see a long laundry list of things, and maybe something will trigger a thought.
Hi Dr Elderman,
I am of Asian Origin. Due to my mum has Diabetes History. I am doing self check thru Glucometer daily. Has not see any doctor for any blood sugar test. I am 43 of age, I am doing my own weight reduction and food planning since last year. I am 163cm in height. I have drop 17kgs since last March 2020. My weight now is 91Kgs and myself is aiming for 70kgs weight. I am doing walking after meal for at least 30-45mins a day usually after dinner. I am doing I.F and skipping breakfast. My fasting morning reading usually in the range of 5.7-6.3. post meal usual range 4.8 to 5.8. after meal 2hrs sometimes in high reading of 10.3 to as low as 6.9. When in high reading, I retake the test again 15mins and 30mins after the 2hrs mark and it did drop very fast back to 7 to 8 range. Is this normal?
It sounds like your numbers might be slightly above normal and you might have pre-diabetes. It’s nothing to panic over though and it sounds like you are doing everything right, but you should get an A1c test.
I actually have one of your books,
Think Like a Pancreas. You truly make things clearer. I have had 2 throidectomies and am a type 2, so perhaps that complicates matters? I am a visual artist,a colored artist portaitist, and this illness has taken away my focus and concentration, and I have been under too much syress and anxiety. Thanks for your research and explanation.
Hi doctor I m 34 yrs old Asian male.my blood sugar at morning always around 5.4 to 6.0.and at 45 minutes it’s go until 12mmol with high carb .then at two hours it’s go down to 7..isit normal or I am in problem.i have high cholesterol too.
It’s very normal. The good news is you come down pretty quickly, because what matters is how long you stay high. It’s pretty typical and has nothing to do with cholesterol. Reducing the carbs in your breakfast would help, but nonetheless you’re doing well as you are.
Hello
Hope all is good with you! I’m from Pakistan and my name is Afnan.
Few weeks ago my blood suger is 85 but after consuming 106 grams suger from coke it goes 190 and then return after 2 hours 121.
Yesterday I eat lunch and after one hour my suger level is 109 and two hours still 109 but third hour it goes 144 then drop 120 within one hour without eating anything. What is cause and is this normal my latest hba1c 5.2 yesterday and its still coming from june13.
Please answer.
Totally normal, and stop drinking regular Coke!
Thank you! May God gives you a very good health, wealth and spirit.
Hello doc, After eating dinner my blood suger in 135 2 hours mark but increase again after smoking and chewing tobacco 150 then again drop. My Hba1c is 5.2 from last one year and fasting suger is 85.
Do you have a question, Rehan?
Yes does it normal as above mentioned like my blood suger spike after eating 100 grams 170 then after 2 hours it is 135 but when i smoke cigarette and chewing tobacoo my suger again spike at 150 but after that its come down again like 30 mints 127. Is this normal.
My hba1c 5.2 from last one year and fasting blood suger 85. No diabetes in history not a problem in mother, father, sister and brother.
You aren’t diabetic. Smoking and chewing tobacco should not make a difference if you’re eating the same amount of food with or without the tobacco. Your blood sugar can go up to 170 without having diabetes.
I have a question about postprandial spikes. Can medications like Ozempic and Trulicity delay a postprandial spike? I seem to stay fairly steady after a meal and spike at the 2 1/2 to 3 hour mark. I currently take Ozempic 2 mg, along with other daily diabetes medications. My most recent A1C was 6.9. I know the GLP-1s delay gastric emptying making me wonder if they also delay glucose absorption from food. The 3 hour spike has been my typical pattern for quite a while now and of course the level of spike goes along with what kind of food I eat.
First of all, congratulations on your excellent A1c! Drugs in the GLP-1 class, such as Ozempic, do flatten out postprandial blood sugar, but do not normalize them. This is through several mechanisms:
1. Stimulate insulin secretion
2. Suppress glucagon that is typically inappropriately elevated after eating
3. Delay the absorption of food
At this point it looks like you’re doing fine and you don’t need anything else. Expect a bump after eating, but don’t get too concerned about it.
I am a67yr old tyoe1 x48 years. Pump therapy. A1C’s consistently 5.2-5.6 over many years. Just started using a DexCom. My pre meal bs’s 70-100, 2 hr PP ‘s 130-150. But my BS’s remain 140-160 for 3-5 hours afterwards. Why am I spiking so late after eating ?
First of all, if you call that a spike, you’re doing pretty darn well. That’s better than the average spike for most people. It could be the nutrients that you’re eating (more protein and fat), and also having diabetes for as long as you have, it could be a little bit of gastroparesis.
Hello Dr. Edelman,
Hope you are doing well!
I’ve two questions, yesterday I eat dinner and after two hours my blood suger is 145 mg d/l and third hour 120.
Today I eat lunch with 400 ml sprite 1st hour my blood suger is 109, 2nd hour 114 3rd hour 121 and four hour 101.
Fasting blood suger is 80 to 95 in between, hba1c is 5.2.
Is this normal?
I’m sorry for not introducing my self, I’m from Pakistan my age is 32year, no history of diabetes. Father and mother also doesn’t have diabetes.
With those numbers, it would not appear that you have diabetes.
So totally normal?
Yes.
Hi, can you provide a link for more information on hypoglycemia management? I have been told I have reactive hypoglycemia, and am frequetly below 70; especially at night and during exercise.
Hi my name is Keith and I am 69yrs old. After a life of high physical activities rugby judo army pti etc. At the age of 55yrs onwards I was diagnosed with type 2 pre diabetic. This was caused by not adjusting my weight 130kg so with regular blood test and other things you get out through hence the pre diabetic. I researched food and realised that I was eating a lot of processed food types. I changed my diet to something grilled (mainly chicken) a sliced fresh tomato and olives, this became my staple diet. I lost approx 15kg within a month so I kept up the diet but sometimes I crack and have other things. I now keep a record of my food intake and test frequently for BS levels and like many responses I’ve read on here I get a spike upto 7.2 2hrs later. However when it dies down it drops to under 4. I have learned from the comments that eating big meals has an effect so my question is if I eat little and often would this be a game changer for me? I haven’t looked at your website yet but your advice and recommendations prompted to comment so thank you for that.
Hi Keith,
YES, because you won’t have the spike.
New to this world but I seem to have the opposite problem and I have to use minimum amount of meal time insulin and even then my blood sugar still drops rapidly and it scares me every time.
Talk to your doctor – you may be going through a honeymoon period. I would really hold off or reduce your dose to avoid hypo.