- Type 2 diabetes is a common and complex condition that’s influenced by a mix of factors including genetics, age, ethnicity, hormones, stress, and lifestyle.
- Your body still makes insulin (the hormone that helps move sugar from your blood into your cells), but it either doesn’t make enough of it, or your cells don’t respond to it properly because of insulin resistance.
- Lifestyle matters…eating balanced meals can help keep your blood sugar steady, and you don’t have to give up everything you love. Exercise is also important and can help to lower blood sugar, make insulin work better, and lift your mood.
- Metformin used to be the go-to treatment for type 2 diabetes, but newer medications like GLP-1 receptor agonists and SGLT2 inhibitors often take center stage now because they can address multiple health conditions including obesity, kidney disease, and heart disease.
- Complications like nerve damage, kidney disease, heart disease, and vision problems can happen, but keeping your blood sugar in a healthy range as much as possible goes a long way in lowering your risk. Since type 2 diabetes can go undiagnosed for years (there aren’t symptoms in the early stages) it’s important to screen for these complications when you are first diagnosed.
Reading Time: 7 minutes
Just received a type 2 diabetes diagnosis?
Getting diagnosed with diabetes can stir up a whole swirl of emotions. You might feel overwhelmed, confused, frustrated, or maybe even a little ashamed.
So let’s clear something up right away – this is not your fault! Type 2 diabetes is a complex condition influenced by many factors outside your control. Lifestyle plays a role, but so do genetics, ethnicity, age, hormones, and even stress.
Whether you had a hunch something was going on or this news came out of left field, know you’re not alone. How common is type 2 diabetes? More than 38 million Americans have diabetes (that’s about 1 in 10), and the vast majority – 90% to 95% – have type 2 diabetes.
Roughly 6,000 people are diagnosed with type 2 diabetes in the U.S. every day. The good news is that diabetes is manageable, and you have more control over it than you might think.
Here are 10 key things to do and know in the days, weeks, and months ahead.
1. Learn What’s Going On in Your Body

In type 2 diabetes, your body still makes insulin (the hormone that helps move sugar from your blood into your cells), but it either doesn’t make enough and/or your cells don’t respond to it properly. This is called insulin resistance.
As a result, glucose hangs out in your blood instead of getting used for energy, which leads to high blood sugar. This is called hyperglycemia. Over time, hyperglycemia can damage your eyes, kidneys, nerves, and heart, but when you keep your blood sugars in a healthy range, you can lower or eliminate a lot of those risks.
Many folks with a new type 2 diabetes diagnosis also have metabolic syndrome, which is a group of health conditions that include:
- Abnormal cholesterol levels (primarily high triglycerides and low HDL)
- High blood pressure
- Central/abdominal obesity (belly fat)
It’s important to address and treat each of these conditions, because each of these factors leads to a higher rate of heart disease in people with type 2 diabetes.
2. Understand the Numbers that Matter
After a type 2 diabetes diagnosis, you’re going to hear a lot about “your numbers”. These are like the vital signs of diabetes management – key data that give you and your care team a clear picture of how things are going.
Here are some of the most common numbers to know:
- A1c: This is your average blood sugar over the last 2–3 months. The A1c goal for most people with diabetes is usually under 7%, but individual goals vary. FYI, your labs will show “normal” levels which are for people without diabetes, so don’t think your A1c should be below 5.7%!
- Fasting blood glucose: This is measured when you haven’t eaten for 8 hours. The target is between 80–130 mg/dL. In your labs it will say less than 100 mg/dL, but that’s not for people with diabetes, so don’t freak out!
- Post-meal blood glucose: This is your blood sugar 1–2 hours after eating. The target is usually under 180 mg/dL.
- Blood pressure: The target for most people with diabetes is usually below 135/85 mmHg.
- Cholesterol: Cholesterol goals for most people with diabetes are:
HDL: The higher the better. Over 40-50 mg/dL is good.
LDL: Less than 70 mg/dL, and less than 55 mg/dL if heart disease is present.
Triglycerides: Less than 150 mg/dL (fasting).
Think of these numbers like the dashboard indicators on your car – you don’t have to obsess over them 24/7, but you do want to know if something’s about to overheat. Logging your blood sugar (through an app, on paper – whatever works) helps you and your care team notice patterns.
3. Find a Knowledgeable Care Team

Depending on how complicated your type 2 diabetes is, you may not need to see an endocrinologist. However, a lot of people like to see one once a year just to make sure they’re getting the most up-to-date medications and tests that primary care doctors may not be privy to.
Your healthcare team may include one (or all) of the following:
- A primary care provider
- An endocrinologist or diabetologist (diabetes specialists)
- A Certified Diabetes Care and Education Specialist (CDCES)
- A registered dietitian or nutritionist
- A mental health professional who can provide emotional support if you need it
These folks can help you build a personalized care plan and help you troubleshoot any challenges that come up. Don’t be afraid to ask questions, speak up if you’re confused, or request referrals if you need them.
4. The Type 2 Diabetes Diet: You Don’t Have to Give Up All the Foods You Love

There’s no one-size-fits-all type 2 diabetes diet. A healthy eating plan is an important part of managing diabetes, but you don’t need to break up with bread or swear off cookies for life. Instead, focus on building a balanced, nourishing way of eating. If you’re not sure where to start, that’s when a nutritionist, dietitian, or CDCES can be a big help.
Quick tips:
- Fill half your plate with non-starchy veggies, a quarter with lean protein, and a quarter with quality carbs (whole grains, starchy veggies, legumes, etc)
- Learn which foods spike your blood sugar (everyone’s different)
- Portion size matters (a loaf of cheesy garlic bread doesn’t count as one serving, but we wish it did!)
- Hydrate with water or unsweetened drinks (diet soda is fine if you need the fizz)
If you enjoy indulging in adult beverages, watch our video on alcohol and diabetes to learn how alcohol impacts blood sugar (and how many drinks it takes for endocrinologists to lose their shirts).
5. Exercise for Type 2 Diabetes: The Free & Legal Mood-Boosting Drug

Staying active is one of the best things you can do to manage type 2 diabetes. Exercise helps lower blood sugar, improve insulin sensitivity, reduce stress, and boost mood. And it doesn’t have to mean running marathons (or even running at all).
Here are a few ways to start small in exercising for type 2 diabetes:
- A 10-minute walk after meals (slowly building up the time and distance)
- Gentle stretching or yoga
- Walking in a pool (if there is water in it!)
- Dancing around your living room (clothing optional)
- Gardening (even marijuana if legal in your state!)
Pick something you enjoy, as you’re more likely to stick with it.
A lot of people with diabetes have underlying heart disease when they’re diagnosed, so don’t go starting CrossFit without talking to your provider first. Ask for your doctor’s recommendations regarding the duration and intensity of exercise, and how to build up gradually. He or she may order a test on your heart first, like a treadmill stress test or cardiac echo.
6. Type 2 Diabetes Medications Like GLP-1s and SGLT2s are Game-Changers

The go-to type 2 diabetes medication for years was metformin, but newer type 2 diabetes medications called GLP-1s and SGLT2s are now becoming the first line of therapy. In fact, the American Diabetes Association recommends starting a GLP-1 or SGLT2 right away if you have diabetes and heart issues.
What are GLP-1s and SGLT2s?
- GLP-1 RAs mimic the natural incretin hormone your body releases when you eat, helping your pancreas work smarter, not harder. They also help lower A1c, reduce heart attacks, and help with weight loss. Examples are Trulicity, Ozempic, and Mounjaro.
- SGLT2 inhibitors work differently – they tell your kidneys, “Hey, let’s ditch some of this extra sugar” and you literally pee it out. They’ve been proven to reduce congestive heart failure hospitalizations and slow kidney disease in addition to lowering blood sugar. Examples are Jardiance and Farxiga.
You can take GLP-1s and SGLT2s together, which is a safe and effective strategy to treat your diabetes and protect your heart and kidneys.
Type 2 diabetes is a progressive condition, so your medication regimen may change over time. If this happens, it’s totally normal and expected.
7. Continuous Glucose Monitors: The Crystal Ball of Blood Sugars
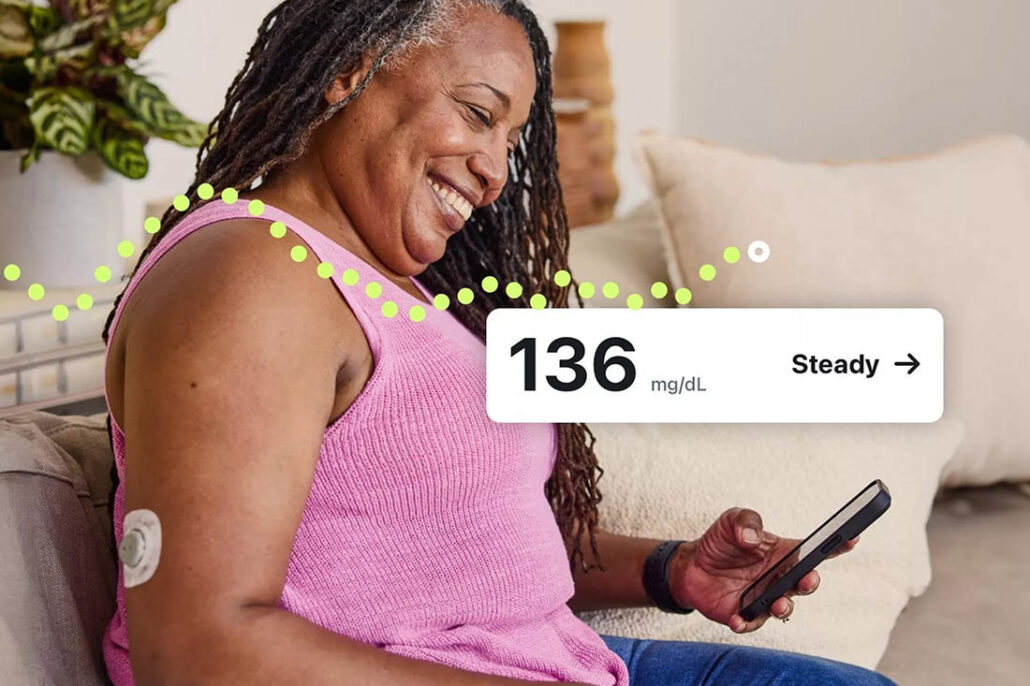
A continuous glucose monitor (CGM) is a small device you wear on your body that tracks your blood sugar 24/7 so you don’t have to prick your finger. It sends blood sugar readings to your smart phone (or a receiver) every 5-15 minutes so you can spot the effects of meals and exercise. Trend arrows can help you catch highs or lows before they sneak up on you. Having these insights can help you make more informed choices that can lower your A1c over time.
If you’re on insulin (even one shot a day), CGMs are typically covered by insurance. If you aren’t on insulin, Dexcom’s Stelo is an over-the-counter option that’s available without a prescription, but you will need to pay out of pocket. Abbott’s Libre Rio CGM will also be over-the-counter when it launches in the U.S.
8. Get Support and Find Your People

Living with type 2 diabetes can be tiring, frustrating, and emotionally draining. Diabetes burnout is real, so make sure you take care of your mental health too.
Here are some ways to prioritize your emotional well-being after a type 2 diabetes diagnosis:
- Connect with others living with type 2 diabetes (through online groups, social media, local meetups, support groups, or type 2 diabetes organizations like Diabetes Sisters or BezzyT2D)
- Talk to a therapist who understands chronic illness
- Be honest with your healthcare provider if you’re feeling overwhelmed
With the right support, managing diabetes and mental health can improve your overall well-being. Diabetes communities can help you feel understood and remind you that you’re never alone in this.
9. Know HOW TO PREVENT Long-Term Complications

Yes, long-term complications of diabetes like nerve damage, kidney disease, heart disease, and vision problems can happen, but managing your blood sugar and keeping it in range as often as you can goes a long way in preventing them.
Other things that can contribute to complications include:
- High blood pressure
- High cholesterol
- Obesity
- Lifestyle (smoking and excessive alcohol intake)
- Genetics (get rid of your parents!)
Regular checkups, screening, staying on top of your care, and taking action early all add up to better outcomes when it comes to diabetes complications. We call these proactive steps the diabetes warranty program. Just like a warranty for your car, if you follow the regularly scheduled maintenance, your car (you) will run better and last longer.
Diabetic kidney disease has no symptoms until there are advanced problems, so screening is important! The two most important tests to get at least every year are the eGFR (which measures how well the kidney is filtering) and the UA/CR (which measures structural damage in the kidneys).
In caring for your heart, keep in mind the following ABCDEs of cardiovascular care:
- A: A1c and Aspirin (in general, A1c less than 7% and 81mg of aspirin/day)
- B: Blood Pressure Control (in general, less than 130/85 mmHg)
- C: Cholesterol Control (see # 2 above)
- D: Drugs (medications to lower cholesterol include statins, Zetia, PCSK9 inhibitors, Nexletol)
- E: Examinations of the Heart (EKG, cardiac echo, stress echo)
10. Ask Questions about Diabetes and Learn All You Can about Your Condition – Knowledge Is Power!
The sooner you take responsibility for your own care, the healthier you’ll be in the long run. Dive into the resources on our website, explore our YouTube channel, join a support group, find a diabetes educator…whatever you do, get yourself educated and don’t solely depend on your doctor to do all the heavy lifting when it comes to your health. They may have the map, but you’re the one driving the car.
Invite your friends and family to be part of your support team, and let them know how they can help you so they don’t unintentionally become the diabetes police.
Frequently Asked Questions
🔄 Is type 2 diabetes reversible?
It can sometimes go into remission, especially with early diagnosis and significant lifestyle changes. But even in remission, ongoing care is necessary.
🩸 Do I have to prick my finger every day?
Not always. It depends on your medications and care plan. Some people use continuous glucose monitors (CGMs), which track blood sugar without fingersticks.
💉 Will I end up on insulin?
Not necessarily—but some people do, especially as diabetes progresses. Insulin isn’t a failure though—it’s just another helpful tool to manage blood sugar.
Dealing with a Type 2 Diabetes Diagnosis: Key Takeaways
Thanks to modern medicine and innovations in technology, managing type 2 diabetes is more doable than ever before. With the right care and treatment therapies, you can dodge a lot of the serious complications that used to be “inevitable.”
Take it one step at a time. Learn the ins and outs of your condition, and ask questions about diabetes. Keep tabs on your blood sugar, blood pressure, and cholesterol, and stick with the TCOYD® crew for the latest research and treatment updates.
People with type 2 diabetes are living longer now than ever before. As clinical diabetes psychologist Dr. Bill Polonsky always says, “The best way to live a long and healthy life is to get a chronic condition and take care of it!” Millions of people are thriving with diabetes, and you can too.
Explore our resource library and video vault for other tips, tools, and support on how to take control of your diabetes.

my doc told me to stop aspirin that it only helps after an incident
Totally not true. Aspirin is for prevention. Get a new doctor. That’s one of the most ignorant things I’ve heard in a long time. (Don’t tell your doctor I told you that!)
been T2 for 25 years. but the last 2 years thanks to my Endo I have all but my weight under control. blood pressure normal and on the lowest dose just for maintenance. cholesterol under control and on the lowest dose statin just for maintenance. off of mealtime insulin. on mounjaro and farxiga with hydroxychloroquine for arthritis. with that my a1c for the past 24 months has been between 5.9 and 6.2 every check.
Wow! That’s awesome, Glenn! Congratulations!!
Thank you for this. I was linked to this article by an acquaintance on the weight watchers website. I’m T2, diagnosed back in 2019, and still feel shame over it. Your advice helps me feel more in control and less isolated.
So glad the article has helped. You are not alone for sure!