
- Optimize your continuous glucose monitor placement: You can wear your sensor in locations beyond the manufacturer’s recommendations, including the abdomen, upper arm, thigh, and lower back. To keep it in place, use adhesives like Skin-Tac, GrifGrips, and kinesiology tape, and consider adhesive removers to avoid skin irritation.
- Make the most of your hybrid closed-loop insulin pump functions: Exercise mode helps prevent lows by adjusting insulin delivery for a higher glucose target, but it can also help avoid alcohol-induced lows and can be used the night before surgery.
- Manage issues from pressure, heat, and altitude: Compression lows can be avoided with easy sensor adjustments. Heat from showers or saunas can cause false highs, and altitude changes during flights can create insulin delivery issues.
Reading Time: 5 minutes
Your continuous glucose monitor and hybrid closed-loop insulin pump can do more than you might realize. Whether you’re a super techie or a technophobe, these diabetes device hacks can help improve your time in range and your peace of mind.
Hack #1: Where to Wear Your Continuous Glucose Monitor
Hack #2: How to Keep Your CGM in Place
Hack #3: How to Avoid Compression Lows
Hack #4: How to Make the Most of Your Exercise Settings
Hack #5: Additional Ways to Use Exercise Mode
Hack #6: How to Prevent Correction Dose Lows
Hack #7: How to Deal with False Highs and Lows from Heat
Hack #8: How to Adjust Your Insulin Pump for Altitude Changes in Flight
Hack # 1: Where to Wear Your Continuous Glucose Monitor
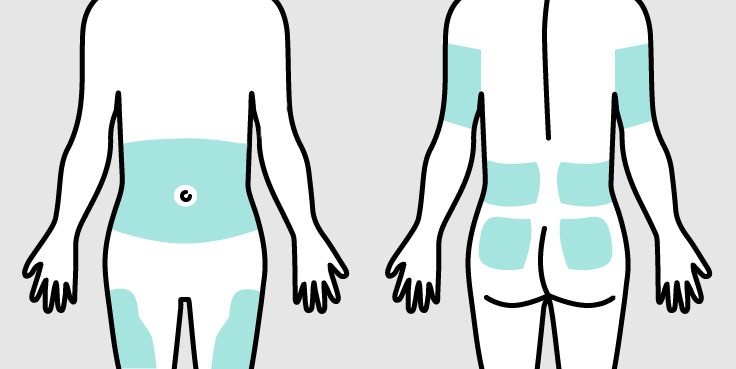
We get asked all the time if it’s okay to wear your CGM in places other than the manufacturer’s recommendation. The short answer is yes! Generally speaking, you can wear your sensor anywhere you have subcutaneous tissue.
Some common locations are:
- The abdomen
- The back of your upper arm
- The upper thigh
- The lower back
- The upper buttocks
CGM companies list guidelines in specific locations on the body because that’s where their sensor placement was studied when they received FDA approval, but other locations can work just as well (and sometimes better).
Hack # 2: How to Keep Your CGM in Place

Have you ever gotten so sweaty that your sensor falls off? We don’t need to know the details, but adhesives can help. Before applying any type of adhesive, make sure you’re putting it on clean skin. Dirt, oil, moisture, and lotions can all interfere with adhesives.
There are lots of different types of adhesive products, including:
Some adhesives can be difficult to remove, so adhesive removers like Skin-Tac or Mirabalm can help protect your skin when you’re taking off your continuous glucose monitor.
Hack # 3 How to Avoid Compression Lows
Compression lows happen when a CGM sensor gets pressed against a hard surface (like a mattress) leading to artificially low CGM readings.
You can usually tell a compression low by a series of steady readings followed by a sharp drop:
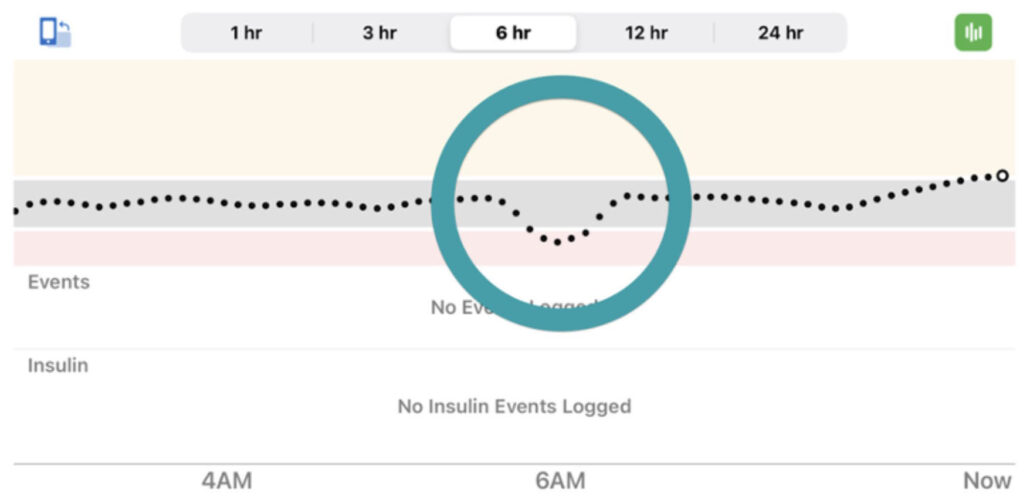
How to manage compression lows:
- Sensor Placement: Be strategic about sensor placement. Avoid putting the sensor on areas that you often sleep on, such as your abdomen or upper arms. Consider placements like the back of the upper arm (if you don’t sleep on it) or the thigh.
- Sleeping Position: If you don’t want to change where you wear your CGM, experiment with different sleeping positions or try using pillows to relieve direct pressure.
- Implantable Continuous Glucose Monitor: You can also try the Eversense 365 CGM, which has an implantable sensor that lasts for a full year. Compression lows don’t happen with this device.
Keep a glucose meter close by your bed so you can double check a low before eating everything in sight (unless you have obvious low symptoms).
Hack # 4: How to Make the Most of Your Exercise Settings

If you use a hybrid closed-loop (HCL) insulin pump system, it has an exercise setting that can really help keep you in range when you’re working out. The setting uses an increased target glucose level and adjusts insulin delivery accordingly to help prevent lows.
A typical goal to shoot for in exercise mode is a higher goal like 150 or 160 mg/dL.
Some systems allow for a percent reduction in insulin administration depending on the intensity and duration of the exercise.
The key is to put your system in exercise mode one to two hours before you start your activity.
Try to remember to turn exercise mode off 20-30 minutes before you stop exercising to prevent a post-exercise rise.
Hack # 5: Using Exercise Settings to Stay in Range During A Night Out & Before Surgery
While it’s primarily used for exercise, there are other times exercise mode can be helpful:
- Alcohol can cause delayed hypoglycemia, especially several hours after drinking. If you’re going out, using the exercise setting may help prevent lows later when you’re sleeping.
- Before surgical procedures: Exercise settings are also often used before surgical procedures, and are usually set at bedtime the night before.
Always check with your doctor before making any changes to your diabetes regimen.
Hack # 6: How to Prevent Correction Dose Lows
There are a few important ways you can avoid going low from a correction dose:
- If you’re about to give yourself a correction dose and your HCL system says “no correction dose recommended”, please take that advice! Some systems are more aggressive than others, and if you ignore its advice you will go low. If you look at the insulin given over the previous two hours (as well as the trend arrow of your CGM) you will see that you already are being automatically corrected by the algorithm.
- Entering fake carbs is another strategy often used to correct for a high. However, if you enter fake carbs, your HCL will still give you your normal basal rate plus the insulin for the fake carbs you entered but did not eat. This can easily lead to hypoglycemia. If you know you’ve under-bolused for a meal, enter carbs a little later to make up for it when you see your glucose rising.
- Inhaled insulin Afrezza can also be used in certain situations to correct for a high. Afrezza gets into your system fast and gets out of your system fast, so there’s less chance for low blood sugars.
Hack # 7: How to Deal with False Highs and Lows from Heat

Taking a hot bath, jacuzzi, or sauna can give you false high glucose values.
If you are someone who has false high blood sugar readings from heat, you might want to temporarily suspend insulin delivery on your hybrid closed-loop insulin pump system before you take a shower, bath, hot tub, etc. If you see high readings when you get out and you’re in doubt, check with a finger stick.
Hack # 8: How to Adjust Your Insulin Pump for Altitude Changes in Flight

A recent study investigated how atmospheric pressure changes during commercial airline flights can affect insulin pump delivery in the following ways:
- During takeoff, a drop in cabin pressure can cause air bubbles to form in the cartridge, which can cause a small amount of extra insulin to be delivered.
- At cruising altitude, rapid decompression (a rare occurrence of sudden loss of cabin pressure) could cause pumps to release too much insulin.
- During descent, the air bubbles dissolve which can pull small amounts of insulin back into the pump. This may lead to blood sugar being higher than usual.
Before takeoff you could try disconnecting your pump, then removing any air bubbles before reconnecting it at cruising altitude about 20 minutes later. For pumps that can’t be disconnected, you may need a small snack to avoid or to treat hypoglycemia after takeoff.
Everyone can be affected differently though, so pay attention to your blood sugars and try to always bring fast-acting carbs in your carry-on.
CGM and Hybrid Closed-Loop Insulin Pump Hacks: The Takeaways
Mastering CGM and hybrid closed-loop technology takes time, but knowing some of the tips and tricks and understanding how to use the devices to your advantage can make a big difference in improving your time in range and quality of life. At the end of the day, it’s all about using this technology to work for you, not against you.
Staying educated and experimenting with what works for you and your lifestyle is key. Joining an online community group is a great way to meet other people and get new ideas on how to live a long and healthy life with diabetes.


Great article! I learned some new techniques, even though I have been on a pump for 30 years. Compression lows and new sensor site locations will be a great help.
Awesome, Roger! Thank you for your comment! 🙂
Thank you! I travel a lot and unexpectedly go LOW a lot! Thank goodness for GU packs.
Last flight I had a GU pack, 4 orange juices plus 4 sugar packs in my last OJ.
Needless to say I felt like crap as eventually I went to 398. And still had another flight. This is not normal for me to go that high.
Thanks for the additional info.
T1D since 2009 (diagnosed at 32)
Omnipod
Dexcom
Loop
GU packets are so convenient for travel! Thanks for your comment, and take good care when you’re flying around up there!
What is a GU packet?
Hi Ann,
It’s an energy gel packet. Super portable with lots of different flavors:
https://guenergy.com/products/energy-gel?srsltid=AfmBOorzOpGWw84RpyGUwOZG9gZVseFptts2bTzYXikvCR5SZfj8Gk4G
My Dexcom 6 typically reads out of range when walking outside and often reads out of range period. Dexcom reports that this is RF interference which they can’t address, and at one point they told me to use another product! It’s concerning not to have sugar readings while exercising (I can easily check blood when at home). Any recommendations for this?
Thanks,
Rebekah
A lot of folks have been seeing the same issue. Sometimes just putting the pump super close to the Dexcom will help. You may need to switch if this does not work.
So glad to see the information about how the pressure changes from flying can be an issue. I’ve suspended my pump and disconnected, and have noticed that a small amount of insulin does come out of the tubing. This can definitely cause low blood sugar, especially for people who are quite sensitive to insulin. I have LADA diabetes and in the early stages was SUPER SENSITIVE to insulin. A half unit was enough to cause a nosedive! Now, I always disconnect my insulin pump from takeoff until we get to cruising altitude. That’s solved this issue.
Thanks for sharing, Lin!