- Think diabetes is just type 1 or type 2? Think again – there are actually over 10 different types of diabetes, with more potentially on the horizon.
- From the autoimmune roots of early-stage type 1, to the genetic twists of MODY, to the newly recognized complexities of type 5 diabetes, they all affect how the body manages blood sugar.
- Research is moving fast, and scientists are continually uncovering new layers to each condition. The more we learn, the better we get at diagnosing and personalizing treatment so you can live your best, healthiest life, regardless of the type you have.
Reading Time: 5 minutes
So you think there are only two types of diabetes? Buckle up – diabetes isn’t just a two-trick pony. There are actually over 10 different types. Some are really common, some are super rare, and some are keeping researchers up at night.
However, they all have one thing in common – they mess with how your body manages blood sugar. Knowing which type of diabetes you have helps guide treatment strategies, so let’s dig in.
1. Early-Stage Type 1 Diabetes (Also Called Pre-Type 1 Diabetes)
Type 1 diabetes doesn’t just poof! appear overnight. It’s actually a slow build-up that happens in stages (we’re talking years), long before your blood sugars start to rise. In these early pre-type 1 diabetes stages, T1D autoantibodies can be detected in your blood. Anyone can be screened for T1D with a simple blood test.
Here’s how it happens:
- Stage 1: Two or more autoantibodies can be detected, but your blood sugar is normal and there are no symptoms.
- Stage 2: Autoantibodies are present, your blood sugar starts creeping up, but symptoms are still generally MIA.
- Stage 3: Symptoms show up in force, blood sugar is super high, and T1D is officially diagnosed.
The T1D antibodies we look for are:
- GAD
- IA-2A
- IAAs
- ICAs
- ZnT8A
Knowing you’re in early-stage T1D gives you time to learn about the condition and explore medications like Tzield that can delay its onset.
Quick Facts:
- Risk factors: Family history, genetic predisposition
- Symptoms: No symptoms in stage 1 or 2
- Treatments: Glucose monitoring, optional clinical trials, Tzield
2. Type 1, Type 1.5 & Latent Autoimmune Diabetes in Adults (LADA)
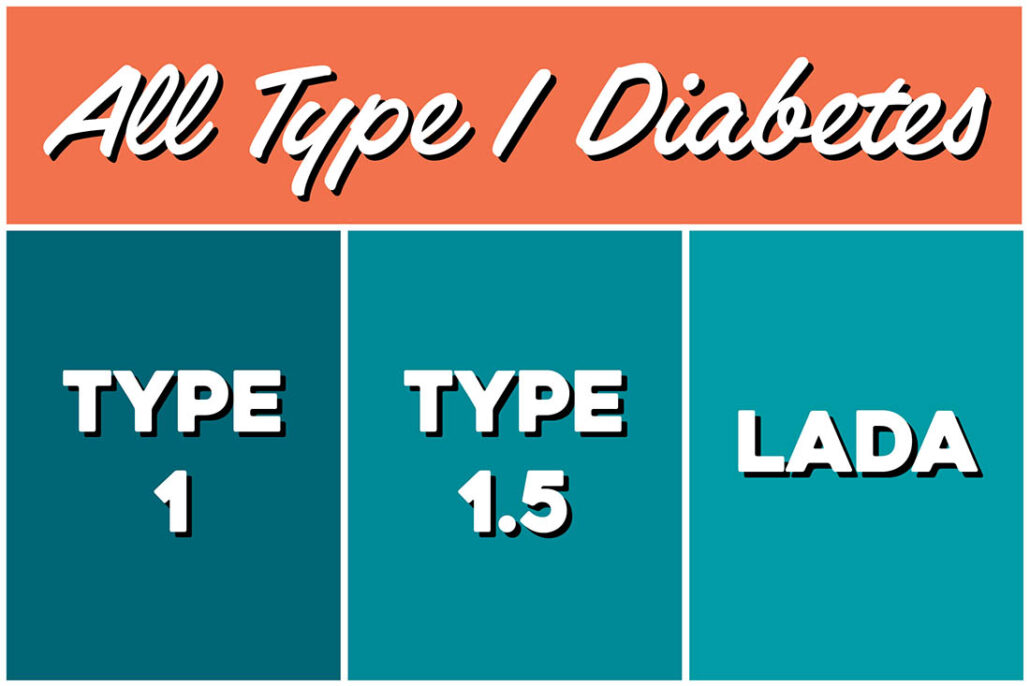
Type 1 diabetes happens when your immune system goes haywire and mistakenly destroys insulin-producing beta cells in your pancreas. We don’t know why this happens, but researchers are working hard to figure it out. T1D can be diagnosed at any age; in fact, more than half of new cases occur in adults.
Which brings us to LADA and type 1.5.
LADA (Latent Autoimmune Diabetes in Adults), also sometimes called type 1.5, is simply type 1 diagnosed in adulthood. Because beta cell destruction can be slower in adults, it’s often misdiagnosed as T2D. Our vote (if anyone’s asking) is to stop using the terms LADA and type 1.5 because they are still type 1 diabetes, and the various terms are confusing.
Quick Facts:
- Risk factors: Family history, genetic predisposition
- Symptoms: Full-blown T1D symptoms include frequent urination, excessive thirst, weight loss, and blurred vision, but in LADA they are more subtle, which contributes to a delay in diagnosis
- Treatment: Insulin therapy
3. Antibody Negative Type 1 Diabetes
Some people have every classic type 1 diabetes symptom, but they test negative for the autoantibodies. Up to 15% of people with T1D fall into this category.
Quick Facts:
- Risk factors: Not well understood, happens in both children and adults
- Symptoms: Same as type 1 (thirst, urination, weight loss, fatigue, etc.)
- Treatment: managed the same way as antibody-positive type 1
4. Prediabetes
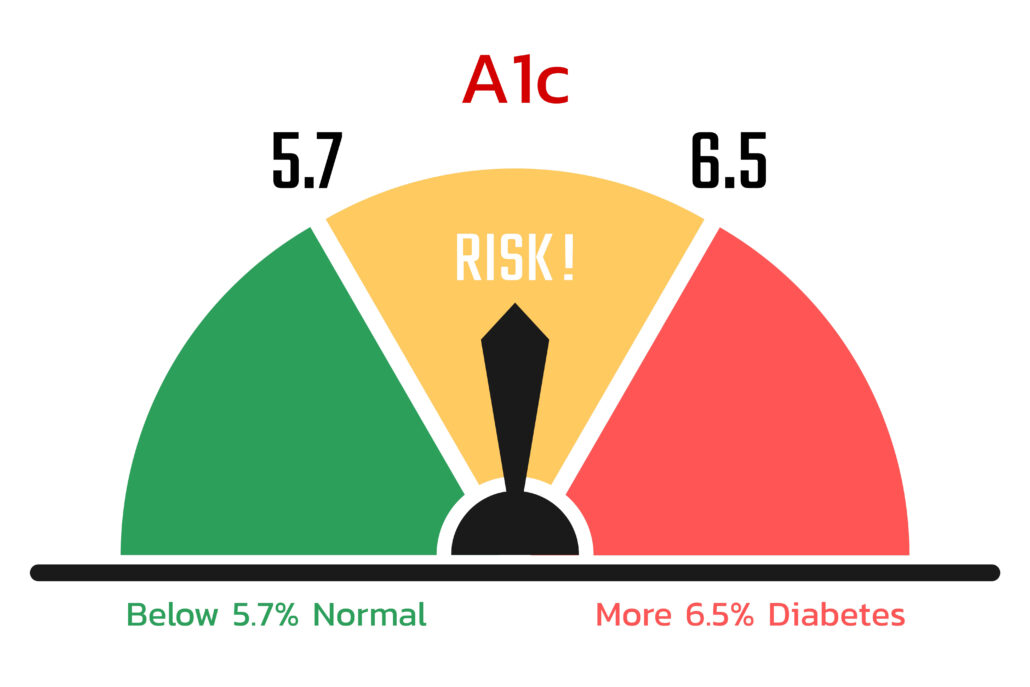
Prediabetes is type 2 diabetes in the very early stages. Blood sugars are higher than normal, but not in diabetes territory just yet. The good news? Progression to type 2 is not inevitable. Prediabetes can often be reversed with lifestyle changes or taking a GLP-1 medication like Wegovy or Zepbound.
Quick Facts:
- Risk factors: Family history, central obesity, high triglycerides, low LDL
- Symptoms: Usually no symptoms – often only found with screening tests
- Common treatments: Lifestyle changes (weight management, diet, physical activity), sometimes metformin or a GLP-1 medication
5. Type 2 Diabetes
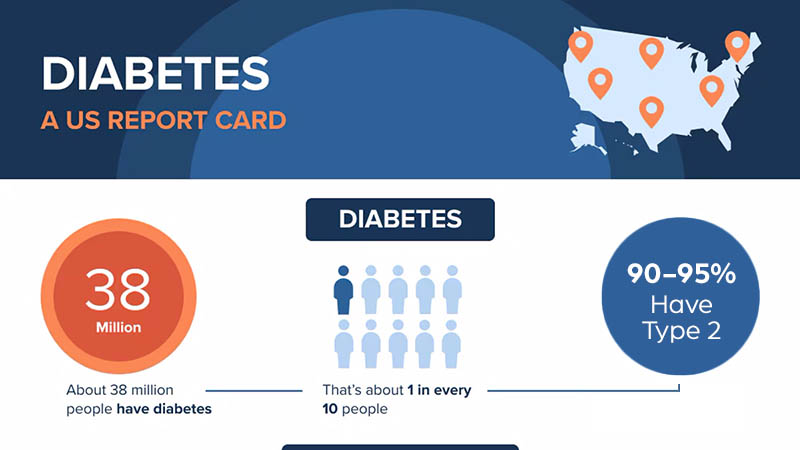
Type 2 diabetes is the most common type of diabetes, affecting over 30 million people in the U.S. alone. Your body still makes insulin, but it either doesn’t make enough of it, or your cells don’t respond to it properly because of insulin resistance. Many people with type 2 also have metabolic syndrome, which is a group of conditions that include abnormal cholesterol levels, high blood pressure, and central obesity.
Quick Facts:
- Risk factors: Overweight/obesity, family history, older age, ethnicity
- Symptoms: Often gradual; increased thirst, frequent urination, fatigue, slow-healing wounds
- Common treatments: Lifestyle changes, oral and/or injectable medications, insulin if needed
6. Gestational Diabetes

Gestational diabetes is a type of diabetes that normally occurs in women. 😉
Pregnancy hormones can make your body more insulin-resistant, which can lead to diabetes. Gestational diabetes usually goes away after the baby is delivered, but during pregnancy it needs to be watched closely to keep mom and baby healthy. If left untreated, it can lead to complications like a larger baby or delivery issues.
Quick Facts:
- Risk factors: Family history, previous gestational diabetes, older maternal age, ethnicity, overweight
- Gestational Diabetes Symptoms: Often no obvious symptoms, usually found through screening tests
- Common treatments: Diet and exercise, glucose monitoring, insulin or oral medication if needed
7. Ketosis-Prone Type 2 Diabetes

Ketosis-prone diabetes (called “Flatbush diabetes” at first, as it was identified in the Flatbush neighborhood of Brooklyn) is a less common form of diabetes that blurs the lines between type 1 and type 2.
People are often diagnosed in DKA, which is typical for type 1 diabetes. However, they can often come off insulin and switch to oral meds once their blood sugars return to normal, which is more typical for type 2 diabetes.
Quick Facts:
- Risk factors: Ethnicity (more common in African American, Hispanic, and Asian populations), overweight, family history of type 2
- Symptoms: Extreme thirst, frequent urination, fatigue, DKA symptoms
- Common treatments: Insulin at first, then oral medications
8. MODY

MODY (Maturity Onset Diabetes of the Young) is a type of diabetes caused by a single gene mutation (also called monogenic) passed down from a family member. There are at least 13 different subtypes, and it typically shows up before age 25.
People with MODY usually produce some insulin, just not enough. MODY can go undiagnosed for years, but a simple genetic test can confirm it.
Quick Facts:
- Risk factors: Strong family history; autosomal dominant inheritance
- Symptoms: Often mild high blood sugar noticed in youth or young adults
- Common treatments: Some require insulin, others respond to oral medication, and some need no treatment at all
9. Type 3c Diabetes
Type 3c diabetes (also called pancreatogenic diabetes) is a type of diabetes that can show up when something damages the pancreas and keeps it from making enough insulin. People with type 3c often have both diabetes symptoms and signs of pancreatic exocrine insufficiency, such as difficulty digesting food.
Quick Facts:
- Risk factors: Pancreatic disease, chronic pancreatitis, cystic fibrosis, hemochromatosis, pancreatic cancer, surgery to remove part of the pancreas
- Symptoms: Increased thirst, frequent urination, fatigue, numbness or tingling in extremities, slow-healing cuts, digestive symptoms like abdominal pain, bloating, gas, diarrhea, fatty or oily stools
- Common treatments: Blood glucose management, pancreatic enzyme replacement, dietary support
10. Type 5 Diabetes

Type 5 diabetes is a newly recognized form of diabetes that’s also known as malnutrition-related diabetes. It develops primarily in children, teens, and young adults who’ve experienced long-term undernutrition. Because of this, the pancreas doesn’t develop fully, so it makes less insulin than the body needs.
The condition is primarily seen in regions with chronic undernutrition, and is estimated to affect 20 – 25 million people worldwide. Researchers are working on the best guidelines for recognizing and treating it.
Quick Facts:
- Risk factors: Long-term undernutrition
- Symptoms: Increased thirst, frequent urination, headache, fatigue, slow-healing cuts and sores
- Treatment: Currently often treated with insulin and nutritional support
Honorable Mentions
We’ve covered the main types of diabetes, but here’s a shout-out to a few of the lesser-known variations:
- Double Diabetes: This is when someone has both type 1 and type 2 diabetes, which can happen!
- Neonatal Diabetes: This is a rare form of diabetes that occurs in infants under 6 months old.
- Type 3 Diabetes: At TCOYD®, we’ve always playfully labeled “type 3s” as friends and family of people with diabetes. However, type 3 diabetes is now a proposed term to describe the link between insulin resistance in the brain and Alzheimer’s disease and other dementias.
- Type 4 Diabetes: This is a proposed term for age-related diabetes that occurs in lean older adults who have insulin resistance. (We used to define type 4s as a previous type 3 who got divorced!)
Frequently Asked Questions
🧐 What’s the Difference between Type 1 and Type 2 Diabetes?
People with type 1 diabetes have an autoimmune condition where their immune system mistakenly attacks and destroys the insulin-producing beta cells in their pancreas, so they can no longer make their own insulin. People with type 2 diabetes still make insulin, but they either don’t make enough or it doesn’t work as well as it should. Many people with type 2 diabetes can manage their blood sugar with lifestyle changes (like healthy eating and exercise) and/or medications.
➕ What should you do if you test positive for type 1 diabetes autoantibodies?
If you have one positive autoantibody, you should be screened every year to see if additional antibodies develop. If you have more than one autoantibody, your lifetime risk of progressing to T1D is nearly 100%. You should get a continuous glucose monitor and have regular checkups to keep an eye on blood sugar levels.
🙅♀️ Can you prevent type 2 diabetes if you have prediabetes?
You can significantly reduce your risk of developing type 2 diabetes with lifestyle modifications like losing weight, maintaining a healthy diet, and getting about 30 minutes a day of moderate physical activity. GLP-1 medications have also been shown to reduce the risk of progression to T2.
❤️🩹 Is there a cure for type 2 diabetes?
There’s no cure for type 2 diabetes (at least not yet!), but it can go into remission. If you lose a certain percentage of weight, your blood sugars might return to the normal range, and you may even be able to cut back (or stop) some of your meds. Some people call this “reversing” diabetes, but “remission” is a better term. Your diabetes isn’t gone, but it’s under control. Just keep in mind that if old habits return, so could your condition.
Understanding the Types of Diabetes: Key Takeaways
The world of diabetes is far more complex than the traditional labels of type 1 and type 2. From the autoimmune roots of early-stage type 1, to the genetic twists of MODY, to the newly recognized complexities of type 5, diabetes isn’t one single disease…it’s a whole spectrum of conditions that affect how the body handles blood sugar.
Knowing which type of diabetes you have shapes how you treat it, track it, and take care of yourself. But no matter which type you have, we are all blood brothers and sisters!
Research is moving fast, and scientists are continuously uncovering new layers to each condition. The more we learn, the better we get at diagnosing and personalizing treatment so you can live your best, healthiest life.
Explore our resource library and video vault, and subscribe to our monthly digital newsletter for more tips, tools, and expert guidance on how to take control of your diabetes.

Our goal is to protect your personal health information. Please keep your questions general and do not post personal medical information here. If you have a specific question, please email events@tcoyd.org.
What about CIADM ( Checkpoint Immunotherapy Acquired Diabetes Mellitus). Currently lumped under Type 1. Does it need an its own category, since immunotherapy is now the Gold Standard for most cancers. Thanks,
That’s really a good point! It’s a common immunotherapy and it can cause what looks like type 1, except there aren’t autoantibodies because it’s not an autoimmune condition. You’re right about that…it should be in it’s own category, but it could also be in the category of autoantibody negative type 1. Thank you for that!
Whatever happened to diabetes insipidus?
It’s back in the Latin dictionary, where it belongs. 🙂
I love TCOYD!
We love you too! 🙂
Such great information. Thank you!
Thank YOU! 🙂
Whoa! Who knew there were so many?! 🤯
Exactly! 🙂
I had several bad allergic rashes from the glue while using the freestyle monitor. Do you know if there has been any changes in the type of glue used? The doctor moved the monitor from my arm to my hip and the same red, oozing rash.
Thanks,
Unfortunately I don’t have any information on that, but check out this article we did on the topic, and read through the ideas people suggest:
https://tcoyd.org/2021/01/__how-do-you-keep-your-cgm-in-place/
You can also reach out to Abbott customer service to see if there has been a change in the adhesive.
I’m a type 1 diagnosed as an adult after the usual misdiagnosis in the US. have a cousin in India who had similar symptoms as me(lean, high BG despite diet and exercise, oral meds not v helpful)and treated as type 2 for years with poor control. But, no auto antibodies, and his insulin levels seem not very low They determined it was LEAN type2 diabetes. Is did find some papers abt it, but not a lot. Any thoughts on treatment options?
About 10% of all type 2s are lean. The lean patients are more insulinopenic, meaning they have less insulin around than heavier type 2s. Treatment comes down to insulin therapy, and adding on other type 2 meds if they are indicated or help, like a GLP-1. The new hybrid closed-loop systems can help too. But obviously it’s important for your cousin to speak with his healthcare provider regarding treatment options.