
Updated 7/28/25
Reading Time: 4 minutes
It doesn’t seem fair – because it’s not – but you can win the lottery you never bought a ticket for and end up with both type 1 and type 2 diabetes, which is also called “double diabetes”. This is because they are two distinct conditions with different etiologies (a fancy word for the cause of a disease).
This case is important to highlight because it has both therapeutic and genetic implications, which are different for type 1 vs type 2 diabetes. Type 2 diabetes is extremely hereditary. Even though type 1 diabetes is less genetic, if you have a close family member with type 1 or any other autoimmune condition, you should get screened for T1D autoantibodies. If you are positive, you need to learn about a medication for people with positive autoantibodies that can delay or prevent the onset of T1D.
There aren’t actual screening tests for type 2 diabetes other than testing glucose levels and A1c occasionally, but you should keep an eye out for the common metabolic syndrome abnormalities that we see in T2D, like high blood pressure, high triglycerides, and low HDL cholesterol levels. You want to be diagnosed early for the best outcomes.
So how does someone get lucky enough to end up with both type 1 and type 2? I’ll walk you through a real-life example from one of my patients.
Type 1 vs. Type 2 Diabetes: What’s the Difference?
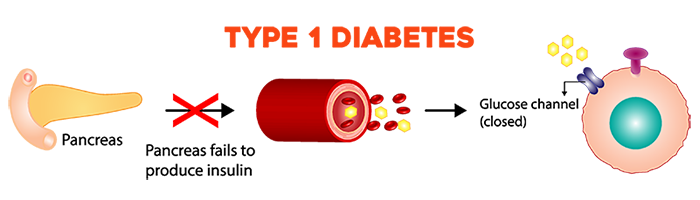
Type 1 diabetes is an autoimmune condition that occurs when the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. It can happen at any stage in life, from infants to older adults. People with type 1 diabetes need daily insulin for life. According to the CDC, about 5-10% of people in the U.S. with diabetes have type 1.
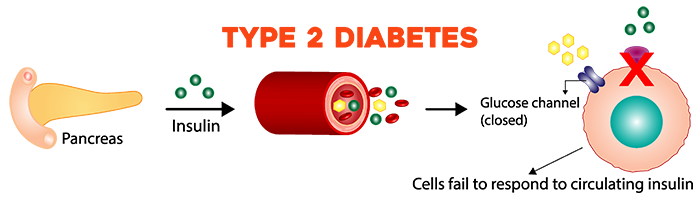
In type 2 diabetes, the body still typically makes insulin, but it doesn’t really work well (this is called insulin resistance) and it’s not enough to normalize the blood sugar. T2D is most commonly diagnosed in adults over 45, but it can occur in kids too. People with type 2 diabetes can do quite well with medications and lifestyle changes. More than 38 million Americans have diabetes (about 1 in 10), and about 90% to 95% of them have type 2 diabetes.
Meet the Patient: Derek
Derek is 62 years old and was diagnosed with type 1 diabetes when he was only six. He presented with DKA (diabetic ketoacidosis) and was hospitalized in the ICU (a common occurrence way back then). He was on MDI (multiple daily injections) for decades because that was really the only treatment available, and he managed his condition as best he could for years with the help of his mom. His A1c was typically in the upper 7% range to the low 8% range. An A1c goal of 7% or under is common for most people.
In 2017, Derek transitioned from MDI to the Medtronic MiniMed 670G hybrid closed-loop system because he was tired of giving himself shots. He did well on the 670G, and after a few months his A1c was in the mid 7% range. Everything was cruising along fine until he hit middle age. Ain’t it the truth for a lot of us!
The Problem: A Strong Family History of Type 2 Diabetes
Both of Derek’s parents have type 2 diabetes. When both of your parents have type 2 diabetes, your chance of getting it at some point is huge – virtually 100%. Unfortunately the gene pool cards were stacked against Derek in this case. In his late 40s, he started to slowly develop the classic symptoms of type 2 diabetes.
Classic Signs of Type 2 Diabetes:
- Weight gain in the abdominal area
- High blood pressure
- High triglycerides
- Low HDL (the good cholesterol)
- Insulin resistance
Because Derek was becoming more insulin resistant from type 2 diabetes, he needed a lot more insulin to keep his blood sugar in range. His insulin requirements went from about 50 units per day to often more than 100 units per day – almost double!
The Game Plan: How to Tackle Double Diabetes
It’s important to note that all of these changes didn’t happen overnight – they occurred over the course of four to five years.
When it became clear that we were dealing with type 2 diabetes in addition to type 1, we started Derek on a typical type 2 diabetes treatment protocol in addition to his type 1 regimen of his MiniMed 670G hybrid closed-loop system:
- Metformin to help manage blood sugars
- Trulicity (one of the first once-weekly GLP-1 drugs) to manage blood sugar glucose values and excessive weight, in addition to protecting him against heart attacks and strokes
- An ACE inhibitor for high blood pressure and to protect his kidneys
- Gemfibrozil (Lopid) to lower his triglycerides
Later we added the SGLT2 inhibitor Farxiga because he started to develop early renal insufficiency, which is not uncommon.
When Mounjaro became available, we switched him from Trulicity to optimize his glycemic control and assist with added weight loss.
In 2023, we transitioned him to the Medtronic MiniMed 780G hybrid closed-loop system to take advantage of its advanced algorithm and improve his time in range.
If You Have Type 2 Diabetes, Can You Get Type 1 Diabetes?
Some people with type 2 diabetes who end up needing insulin will often say their type 2 diabetes “turned into” type 1. While type 2 diabetes is a progressive condition and insulin may be needed for some people at some point, that doesn’t mean that their type 2 diabetes has become type 1. It just means they now need insulin to help keep their blood sugars in a better range. The correct phrase is “insulin-requiring type 2 diabetes”.
Theoretically it is possible to have type 2 diabetes first and then also get type 1; however, those types of patients are not diagnosed and are classified as having insulin-requiring type 2 diabetes.
The Takeaway
Type 1 and type 2 diabetes are unfortunately not mutually exclusive. Just because you have one type of diabetes, it doesn’t protect you from getting the other…although it should!
If you have type 1 diabetes and you’re worried about getting type 2 diabetes due to a family history of the condition, the best thing you can do is kill two birds with one stone (why would you want to kill two birds?) and maintain an ideal bodyweight. Make sure you’re screened frequently (at a minimum once a year) so if you see signs of type 2 diabetes, you can initiate type 2 medications quickly. That will help prevent the progression.
If you are a glass-half-full kind of person, you can look at the benefit of having both type 1 and type 2 diabetes. The upside is that you can get access to all the awesome medications that are only currently approved for type 2 diabetes, and you can get coverage for a CGM. You can use the double diabetes diagnosis to your advantage, as insurance companies have to cover medications for type 2 diabetes, and technology like pumps and CGMs for type 1 diabetes.
(Side note: You can get a CGM covered by insurance if you have type 2 diabetes and you are on at least one shot of insulin per day.)
Double diabetes is actually not that uncommon, and it is important to have a level of awareness about it if you’re at risk. Living with type 1 and type 2 diabetes may be a double whammy, but it doesn’t necessarily mean double trouble. You can absolutely live well with both. But don’t seek out another diagnosis just to impress your endocrinologist!
Visit our resource library and video vault for other tips, tools, and support on how to take control of your diabetes.

Subscribe
Ironically I had an appointment with my Endo yesterday. My normal Endo is on Maternity leave. So when her replacement asked me, “are you T1 or T2 ?,” I was a bit confused? I have been T1 for 44 years – so it was a weird question. My normal Endo identified insulin resistance and I see used to my advantage to get the approval for GLP1 through a new insurance who would not allow for T1. Even though I had been using for 4 years with a flat 6.4 A1C. When she advocated why I had T2 – Express Scripts approved. Sadly weight loss hasn’t followed my GLP1 use – I’d love 10 pds 😉 However my A1C is improved. For some reason when I was asked if I had T2 – it felt like an accusation or maybe I had done something wrong? I wonder if that is common feeling for those of us with T1 who just had it show up one day – not because of lifestyle – so perhaps we feel we are more unique?
It’s possible that you do have type 1 and type 2, I’d go back to the person who was covering for your normal endo and say you are a type 2 or type 1 with insulin resistance so you can get the GLP-1 medications covered by insurance. However, if you didn’t respond with weight loss to a GLP-1, it’s possible you have something called hypercortisolism. You can learn about it here and see if it resonates:
https://tcoyd.org/2024/08/wondering-why-your-diabetes-is-out-of-whack-it-could-be-too-much-cortisol/
It’s easy to test for.
I am definitely a T1 with T2. I use several traditionally T2 medications, but my insurance won’t cover them because I don’t have a T2 diagnosis. Are doctors in the US able to diagnose T1 and T2? Is there some type of restriction on this.. my Endo won’t do it.
Thanks!
I have no problem listing a type 1 and type 2 diagnosis, but what I recommend is putting in the diagnosis of insulin resistance along with type 1, and that very often is what’s needed to get it approved.
Not as unique as you might think. People with Type 1 seemed “HORRIFIED” about 15 years ago when I posted suggestions in various DOCs that we “could” be both many years ago. In the “olden days” Type 2 “used” to only affect older people…older people with hearts and eyes and skin and blood vessels that are facing the challenges of aging. It stands to reason that the pancreas and liver would also feel the affects of aging and make a person more resistant to the actions of insulin. So what is different about a person with Type 1? Our hearts, eyes, skin, and blood vessels are ALSO affected by aging (and by Type 1 diabetes TOO), so why not our pancreas and liver. It kinda creeps up, but I noticed I was using considerably more insulin than I before. Nothing had changed in my diet or exercise but the basal rates were higher, AND the insulin to carb ration had changed. My doctor recommended I take Metformin…and within a month, my daily insulin use was back down, as were my basal rates, and my insulin to carb ratio. I am glad this can be discussed now without Type 1s getting all bent out of shape with the “WE are different from Type 2.”
Your thoughts are very good, and you’re experiencing what a lot of people experience as they get older. Typically people become more resistant to insulin as they gain weight, and the type 1 population is getting heavier these days. It’s also possible that you have a tendency toward type 2, which does come on later in life. But thank you for your thoughts!
So what is the difference between double diabetes and LADA(type 1.5)?
Hi Fay,
Double diabetes is when you have both type 1 and type 2 diabetes, and LADA is when you are diagnosed with type 1 diabetes as an adult. It stands for “Latent Autoimmune Diabetes in Adults”. Hopefully that term will fall by the wayside as it’s confusing – people with LADA just got type 1 as an adult.
This article does a great job explaining the complexity of “double diabetes,” and I appreciate the clear breakdown of treatment strategies. That said, I was surprised not to see any mention of nutrition or lifestyle interventions.
As a diabetes care and education specialist and clinical exercise physiologist, I’ve created a plant-based diabetes program that has helped many clients achieve what the medical community defines as remission from type 2 diabetes—lowering their A1c, reducing or eliminating medications, and regaining metabolic health.
I know Dr. Edelman has explored plant-based nutrition on his podcast and expressed openness to its benefits. I’d love to see that perspective reflected in future articles, as it could really round out the message and empower readers with more options.
Lifestyle is always an issue with any type of diabetes, whether you have type 1 or type 2, or both. Although it wasn’t the focus of this article, you’re absolutely right. Since my next-door neighbor is a big plant-based guy, I’ve started to go that way myself, so thank you for the suggestions.