- A type 1 diabetes diagnosis is a lot to process, but just take it one step at a time – you don’t have to learn everything overnight.
- CGMs and automated insulin delivery systems are like the Batman and Robin of the diabetes toolkit…they are the technology superheroes of blood sugar management.
- You can still eat carbs, have dessert, and drink alcohol with diabetes – just try to enjoy them in moderation.
- Blood sugar rollercoasters (highs and lows) happen to everyone. Mild and moderate hypoglycemia can generally be treated with fast-acting carbs, but severe hypoglycemia may require assistance from another person or intervention with glucagon.
- Find a supportive T1D community, stay educated, and advocate for what you need. Remember to live life first and be diabetic second – give attention to your diabetes without letting it become the focus of your life.
Reading Time: 8 minutes
Just received a type 1 diabetes diagnosis?
It probably feels like you’re getting hit with a firehose of diabetes medical lingo and instructions for devices you never even knew existed. We get it, we’ve been there. But take a deep breath – it will get easier. And one day words like “diabetic ketoacidosis” will roll off your tongue without you even thinking about it!
Since you may have been released from the hospital armed with little more than a vial of insulin, some vague advice about counting carbs, and a figurative “good luck out there” slap on the backside as you were nudged out the door, we thought we’d fill in some of the gaps and diabetes basics.
Here are 10 key things to know and do in the days, weeks, and months ahead.
1. Chill Out! No One Becomes a Diabetes Ninja Overnight

First, give yourself a moment. Or ten. A type 1 diabetes diagnosis might be overwhelming now, but allow yourself some breathing room and take things one step at a time.
Even though type 1 diabetes is a lifelong condition, it’s one you can live well with into old age. Thousands of people with T1D run marathons, raise families, travel the world, start companies (ahem…TCOYD®), become professional athletes, fly commercial airlines, become Elvis impersonators – you name it!
2. Find a Knowledgeable Healthcare Team

In the old days, people had a dedicated diabetes care team, but that’s a little more difficult to come by with the medical system we have today. That said, in addition to your primary care doctor, you should try to see an endocrinologist with an interest in type 1 diabetes. Some endos like to focus on thyroid conditions, adrenal disorders, infertility, etc., so it’s important that you see a diabetes endocrinologist. You should also have annual visits with an ophthalmologist or optometrist who’s experienced in diabetic eye disease.
Other providers who can help with various aspects of diabetes management:
- A certified diabetes care and education specialist (CDCES)
- A nutritionist or registered dietitian
- A mental health professional who can provide emotional support if you need it
- A personal trainer
Your medical team can help you figure out how much daily insulin you need, how to adjust your insulin doses for meals, activity, stress, and illness, how to troubleshoot highs and lows, and how to deal with diabetes burnout or any other challenges you might have. Don’t be afraid to ask questions, speak up if you’re confused, and advocate for what you need.
3. Choose Your Insulin Regimen

Insulin is a hormone that helps move sugar (glucose) from your bloodstream into your cells for energy. Without insulin, your blood sugar shoots up. You’ll need to give your body the insulin it needs – through injections, an insulin pen, or an insulin pump.
There are two main categories of insulin:
- Basal insulin (also called long-acting insulin): This is the background insulin your body needs all day and night to keep blood sugar steady. Unlike mealtime insulin, which works quickly to cover the food you eat, basal insulin works slowly and steadily over many hours.
- Bolus insulin (also called fast-acting insulin): This insulin handles the rise in blood sugar that happens when you eat. You might also use a bolus dose to bring down high blood sugar (correcting for a high). Think of it as the “extra boost” that steps in when your blood sugar needs more immediate help.
The two best basal insulins are Tresiba and Toujeo because neither has a peak (something you do NOT want in a basal insulin), and they only need to be taken once a day.
There are lots of different brands of fast-acting insulin, including:
- Novolog
- Fiasp (slightly faster-acting than Novolog)
- Humalog
- Lyumjev (slightly faster-acting than Humalog)
- Much older “regular” insulins like Humulin R and Novolin R, which are still available (and much cheaper if cost is an issue)
- Inhaled insulin Afrezza, which gets into your system fast and gets out of your system fast, so you have less chance for hypoglycemia
Your doctor will help you determine the most appropriate insulin type, dosage, and administration schedule.
Most people with a new type 1 diabetes diagnosis are put on multiple daily injections right away, but we recommend you consider going on an automated insulin delivery pump system (also called an AID system or a hybrid closed-loop system).
These are insulin pumps that communicate with a continuous glucose monitor (see # 4 below). AID systems can give you the right amount of insulin automatically, helping to keep your blood sugar in range without you having to do all the work yourself.
4. Get a Continuous Glucose Monitor: The Crystal Ball of Blood Sugars
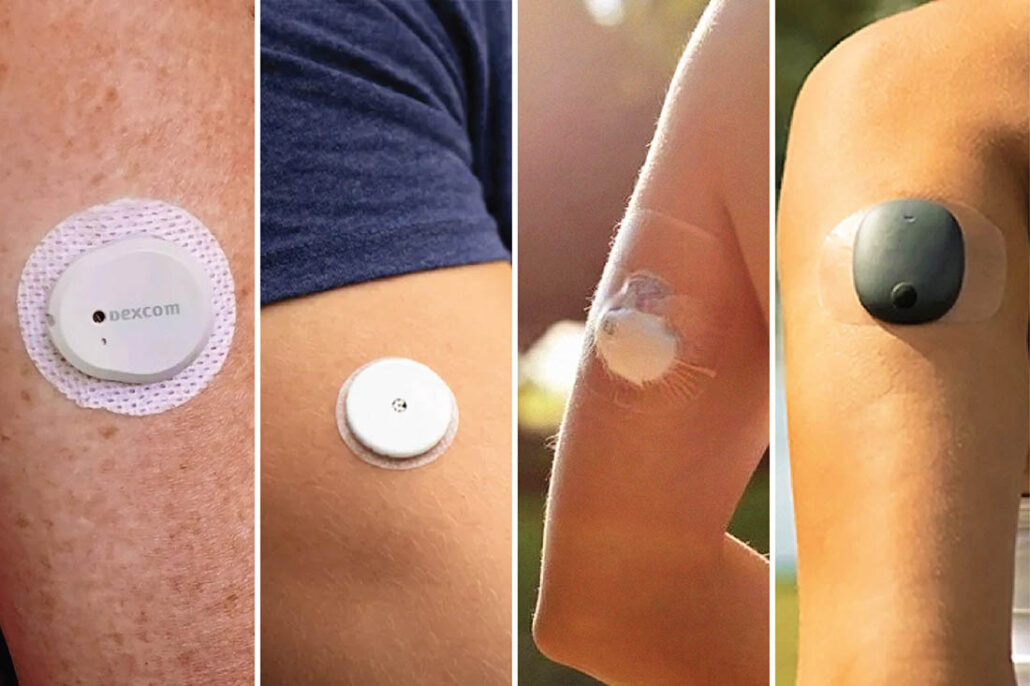
Outside of insulin, a continuous glucose monitor (CGM) is the single most important tool for your diabetes management. It’s a small device you wear on your body that tracks your blood sugar 24/7 so you don’t have to prick your finger. It sends blood sugar readings to your phone (or a receiver), showing you not just where your blood sugar is right now, but also where it’s headed so you can catch highs or lows before they sneak up on you.
CGMs also have alerts and alarms to tell you if your blood sugar is getting too high or dangerously low. You can share your data with your doctor and your loved ones (but not your ex-wife!) if you want to.
Pairing a CGM with an insulin pump can take a lot of the guesswork out of managing T1D and give you more freedom to live your life.
5. Know the Signs of Hypoglycemia and How to Treat It

When your blood sugar is between 70-180 mg/dL, this is what we call “in range.” When blood sugar dips below 70 mg/dL, that’s called hypoglycemia or low blood sugar.
Symptoms of hypoglycemia include:
- Shakiness or trembling
- Sweating (even in a cool environment)
- Hunger
- Fast heartbeat
- Irritability
- Anxiety
- Pale skin
- Headache
- Dizziness or lightheadedness
Symptoms of low blood sugar can vary from person to person – some people may not feel low until their glucose hits 65 mg/dL, while others may start having symptoms at 75 mg/dL.
Generally speaking, mild or moderate hypos can be treated with fast-acting carbs like glucose tablets, jelly beans, apple juice, orange juice, etc.
Severe hypoglycemia typically requires assistance from someone else, and glucagon may be needed.
The newest glucagon options are the Gvoke HypoPen, an injection that can be given in the lower abdomen, outer thigh, or upper arm, and BAQSIMI, a glucagon nasal spray. Since someone else will probably be the one giving you glucagon, make sure your friends, family, coworkers, and teachers know how to use it——and where you keep it.
A blood glucose meter is also important to have if your CGM fails (which can happen) or your physical symptoms don’t match your CGM readings.
While you’re loading things in your Amazon cart, consider getting a ketone meter (with ketone strips) too. Rising ketones mean your body isn’t getting enough insulin, which can lead to diabetic ketoacidosis (DKA), one of the complications of diabetes. Continuous ketone monitoring is on the horizon and will hopefully be implemented into the FreeStyle Libre CGM brand soon, so eventually you won’t need an extra device and strips.
6. Carbs and Cocktails Can Still Be on the Menu

Yes, you can still eat carbs after a type 1 diabetes diagnosis, but most people find that eating low-carb (ish) makes managing diabetes a lot easier. You’ll have to find what works for you. This is when a nutritionist, dietitian, or CDCES can be a big help. There are also a lot of apps out there that can help you determine the amount of carbs you’re eating.
In reality, counting carbs usually ends up being more of a WAG (wild-ass guess) than an exact science, even for people who’ve had diabetes for years. Eventually, you’ll learn how different foods affect your blood sugar, and you’ll get better at predicting the amount of insulin you need. Giving yourself a bolus of insulin about 20 minutes before you eat can really help with post-meal blood sugar spikes.
If you like to partake in adult beverages, watch our video on drinking with diabetes to learn how different types of alcohol can impact blood sugar (and how many drinks it takes for endocrinologists to lose their shirts).
7. Everyone Rides the Blood Sugar Rollercoaster…We’ll Save You a Spot!

Blood sugar levels can go up and down for all kinds of reasons besides food – like exercise, stress, sleep, hormones, heat, someone giving you side-eye at the grocery store – you get the idea. Don’t beat yourself up when your numbers bounce around. It’s totally normal, and it happens to everyone with diabetes.
There are a few tricks of the trade that can help control blood sugar spikes after eating and manage blood sugar during exercise, including insulin timing, splitting your meal, and adjusting your pump settings.
8. Join a Diabetes Support Group and Find Your People

T1D can feel like you’re living on an island all alone, but there’s a huge community of people around the world who are all in the same boat. Connect with others on social media, through national organizations like Breakthrough T1D, in local diabetes support groups, through type 1 diabetes adventure experiences, and at in-person events like our annual ONE Conference and Retreat. There are an estimated 9.5 million people with T1D globally, so your chances of finding a new diabuddy are pretty good!
T1D communities can help you feel understood, offer tips and emotional support, offer advice on diabetes burnout, and remind you that you’re never alone in this.
9. Know the Long-Term Diabetes Complications (and How to Prevent Them)

When you’re newly diagnosed, the scary stuff (like diabetes complications) isn’t something you need to lose sleep over. Complications usually take years and years of consistently high blood sugars to develop.
Still, it’s smart to know what’s on the list: things like nerve damage, kidney disease, heart issues, and vision changes. The good news? Keeping your blood sugar in range as much as possible offers major protection against all that.
Other things that can contribute to complications of diabetes include:
- Blood pressure
- Obesity
- Lifestyle (smoking and excessive alcohol intake)
- Genetics
- Exposure to toxins and dyes, chemotherapy, and vitamin deficiencies
Regular checkups, screening, staying on top of your care, and taking action early all add up to better outcomes when it comes to diabetes complications.
We call this the diabetes warranty program. Just like a warranty for your car, if you follow the regularly scheduled maintenance, your car (you) will run better and last longer.
10. Learn All You Can about Your Condition – Knowledge Is Power!
Type 1 diabetes isn’t caused by eating too much sugar, and you didn’t do anything wrong to “get” it. It’s an autoimmune condition that happens when your immune system mistakenly attacks and destroys the insulin-producing beta cells in your pancreas.
When you take responsibility for your own care early on, the better your health is likely to be. Take a deep dive into the articles and videos on our website, explore our YouTube channel, join diabetes support groups, find a diabetes educator you click with…whatever you do, get yourself educated and don’t solely depend on your doctor to do all the heavy lifting when it comes to your health.
Bring your friends and family into the loop too, and let them know how you would like to be supported. Having at least a few people in your circle who understand what T1D is (and what to do in case of a low blood sugar emergency) can give you peace of mind and be a boost when you need it.
Frequently Asked Questions
🍭 Can I eat sugar with diabetes?
Yes, you can generally eat anything you want. You just need to account for the carbs, which is a lot easier to do now with automated insulin delivery systems. With time (and trial and error) you will learn how to dose insulin for meals and snacks…and yes, dessert!
💉 Will I have to take insulin forever?
Yes, unless there’s a major breakthrough or cure.
👯♂️ Is type 1 diabetes the same as type 2?
Nope. Type 1 diabetes is an autoimmune condition and requires insulin from the start. In type 2 diabetes, the body still typically makes insulin, but it doesn’t work very well (this is called insulin resistance) and it’s not enough to normalize the blood sugar. People with type 2 diabetes are often treated with medications and lifestyle changes.
👫 Is type 1 diabetes hereditary?
Type 1 diabetes does have a genetic component, meaning that if one first-degree family member has the condition, others are at higher risk. The majority of people diagnosed have no family history of the disease, but those who do have a family member with type 1 have an increased risk (up to 15x) of developing it. Type 1 diabetes screening can help relatives take proactive steps.
Dealing with a Type 1 Diabetes Diagnosis: Key Takeaways
A type 1 diabetes diagnosis is a lot to process, but it’s also totally manageable. Is it fun? Not unless you get the opportunity to dress up and sing about it. But your life isn’t over, and believe it or not, diabetes can actually lead to some pretty amazing things.
Try to find a healthy balance between giving attention to your condition without letting it become the overwhelming focus of your life. Yes, you may need to plan ahead a bit more, but diabetes doesn’t have to stop you from doing the things you love.
People with type 1 diabetes are living longer now than ever before. As clinical diabetes psychologist Dr. Bill Polonsky always says, “The best way to live a long and healthy life is to get a chronic condition and take care of it.”
You’re going to be okay.
So stay educated, advocate for what you need, and know that managing diabetes is a marathon and not a sprint. Unless you’re this kid, and then it’s both!
Visit our resource library and video vault for other tips, tools, and support on how to take control of your diabetes.
Additional Resources:
- 50 Secrets of the Longest Living People with Diabetes
- Automated Insulin Delivery Systems: Which One Is Right for You?
- Dissecting CGM Downloads
- How to Improve Your Time in Range Solely by Adjusting Your Alerts and Alarms!
- The Many Reasons for High and Low Blood Sugars (and why we need a LOT of compassion for ourselves!)
- Newly Diagnosed with Type 1 Diabetes? 3 Tips from a Therapist Who Gets It!
- Staying In Range Before and After Exercise
- The Diabetes Warranty Program: Get On It!
- New to type 1 or Haven’t Gotten It Figured Out Yet?
- The Only Type 1 Lecture You’ll Ever Need
- Top 10 Tips to Stay Cool with Diabetes, Part 1
- Top 10 Tips to Stay Cool with Diabetes, Part 2

Weight loss a huge problem! First diagnosed 4 yrs ago as LADA and Rx for metform. Then strict Keto and clean diet and lost 83 lbs. 3yrs ago put on insulin (tresiba and Novolog) as my pancreas stopped producing and consequently within a year gained 50 lbs! I watch thediet as a Type 1 Impossible to take off the weight! Help !
I doubt that starting insulin affected your own endogenous production, but for sure contributed to the weight gain. This is why we use GLP1s in T!D! Talk to your doctor about Wegovy or Zepbound if your BMI is over 27.
This was honestly the kind of guide I wish I had on day one—real talk, practical tips, and just the right amount of humor to make it less scary. It’s a reminder that while T1D is serious, it doesn’t have to take over your life.
Exactly! 🙂 Appreciate your comment!
Wow, the immune system, what a fickle beast! Learning about type 1 diabetes feels like navigating a complex maze. I remember once, feeling completely overwhelmed trying to troubleshoot a software glitch, convinced I’d broken everything myself when it was a deeper system error. Educating yourself, it’s truly the key, isn’t it? Having support around you is huge too. I’d share that experience, it was quite a slippery Slope to climb back up.
We are big believers in staying educated and getting support when you need it! 🙂
Great